Good Practice in the Care of People Of Disability Who are Bed Bound.
July 2021

This page details good practice in the care of People Of Disability who are bed-ridden (temporarily or permanently) for any reason. It is relevant to all those people (professional or amateur), who perform some type of caring service on behalf of persons of disability (nurses, carers, therapists, support workers, assistants, parents, husbands, wives, family members, friends, volunteers, or any other person I have omitted in this list). It may even hold some relevance to those working in special education, particularly residential special education. This page details observations of my experience as a newly disabled person both in hospital and at home following my discharge from hospital. I also think that it might be relevant to other POD especially IRON POD (continue reading for an explanation of those two words). If that applies to you, please contact me and let me know what you think.
I kept copious notes throughout my first year. This page is the result. If you would like to comment on any aspect of this web page, there is a form situated at the bottom of this page for this purpose. This page is dynamic, not static, in that I am continually adding to it as new issues arise or there are further developments in existing points made. To indicate any new additions, I will include a date and, if an update, the word 'update'.
|
I am a disabled man in my late sixties. A year ago, in August 2020, I had a major stroke that put me in Kings Mill Hospital for several weeks. The stroke left me with a left hemiplegia, paralysed completely down the left-hand side of my body and very weak core muscle strength. It also meant that I was doubly incontinent and was fitted with a catheter. Full-time catheterisation meant that I was prone to bladder infections (which are not pleasant). It seemed that I was on a permanent prescription for bladder and urinary tract infections and the antibiotics added to the volume of pills and potions that I had to swallow every day. The problem is that, following the stroke, I found swallowing difficult and would often choke when eating or drinking.
|
Thus, I had to have all my drinks thickened and avoid certain foods. The stroke also affected my speech and talking became something of an effort. Indeed, if I am emotional, or in pain, or my throat is dry, or I am not feeling well, or for reasons unknown, I cannot speak at all and have to resort to using Makaton sign language or my V-Pen and board (more on communication later on this page). As if not all that was enough, I found myself having to cope with lengthy periods of pain and poor post-hospital provision. All of this was during the Covid lock-down, which further compounded my nightmare. Having a stroke made me feel like Gregor Samsa, the salesperson in Franz Kafka’s surreal book (‘The Metamorphosis’: Die Verwandlung. Original in German, 1915), awakening one morning, only to discover that he had inextricably transformed overnight into a very different, somewhat repulsive, being. I awoke, knowing I would have to learn to deal with a new reality; one in which many people might view and treat me differently from now on.

On leaving hospital, I was provided with a manual wheelchair, a hospital style bed, a mobile hoist and sling, a commode (which I have never been able to use for its intended purpose), and a very poor quality over-the-bed style table that I used for just a few days before purchasing a much better version from Amazon. An interim care package with A.M.G. was set up for me that involved four calls during a day but this provision only lasted for a short time until circumstances forced my wife to set up our own system of care. Such service provision was quite difficult to set up and proved to be frighteningly expensive. Having worked all my life and saved for retirement, no financial assistance for support was available; my retirement savings had to be used to cover all the cost of care. Yet, if I did not bother to plan for retirement, and had no savings, then the cost of care would have been virtually covered and the service almost free. My wife is planning on giving up work to help with my care very soon (Visser-Meily, Post et al 2009; Cameron, Cheung et al 2011; Cameron, Stewart et al 2014; Bastawrous, Gignac, et al 2015). She cannot cope with a job and having to meet my needs during the evening and the night. We applied for an Attendance Allowance; to offset some of the income we were losing, only to find that on the maximum level to which we were entitled is £89 per week. Further, my wife is entitled to a Carer’s Allowance of approximately £60 per week. These allowances, plus my state pension, barely cover the cost of the level of care (Rajsic, Gothe et al 2019) that I now need on a daily basis. However, I am truly grateful for the help that I received. I am aware that, in other countries, I would not be provided with anything at all and would have to pay for every little bit of support. I thank the gods that I was born in the UK. We finally settled with a Care Company called Green Square Accord who appeared to meet our needs.
All my working life, I was involved, in one way or another, with People Of Disability (POD) and or learning difficulties. I also was involved in the provision of training for professionals and support workers. I worked alongside gifted Speech and Language Therapists, Occupational Therapists, and Physiotherapists as well as many talented teachers and support staff in many different countries. The focus of the training I provided concerned good practice in education and support provision for staff working with individuals experiencing special needs. It now seems somewhat ironic that I am in need of that support myself! The irony is not lost on me. I had become an I.R.O.N. (Individual totally Reliant on Others for Needs) P.O.D. (Person Of Disability). In POD, the Person comes before the disability but the use of 'of' suggests that the disability defines the Person. Still, the Person comes first, the disability second. I am a POD. What type of POD am I? I am an IRON POD. In IRON the Individual comes first. The Reliance upon Others follows. Needs comes last but defines the Individual, an Individual with needs. The needs are supplied by Others. Thus, putting it all together, it assembles as IRON POD.
|
The level of care provision both in hospital and in post-hospital settings varies wildly from the incredibly good to the unbelievably poor and, as an IRON POD, I thought that I should put down in print my experience and thoughts on the care I have received. What would I consider best practice? (MacKenzie, Creaser et al 2017) I should have some insight, after almost a year of daily care and a little, rather inadequate, post-hospital provision. When a person is ill, the last thing about which they should be worried is the level and standard of care provided. However, the realisation soon comes that, for Individuals totally Reliant on Others for their Needs (IRONs), the standard of care provided plays a major role in an individual’s quality of life (Mayo, Wood-Dauphinee et al 2002; Opara & Jaracz 2010; Van Mierlo, Van Heugten, et al 2016; Caro, Mendes et al 2017)
|

As an IRON POD, I soon came to realise that my future was forever changed. I would, short of some miracle, always be totally reliant on the kindness of others and, if that kindness was, for some reason, to fade and the others chose to walk away, I would be helpless, trapped inside my own body: an IRON POD, a prisoner in virtual irons created as the outcome of a stroke. I understand why so many, in my position, become depressed and even suicidal (Parikh, Eden et al 1989; Parikh, Robinson et al 1990; Van de Weg, Kuik, et al 1999; Kneebone, & Dunmore 2000; Pohjasvaara, Vataja et al 2001; Berg, Palomaki et al 2003; Cassidy, O'Connor, & O'Keane 2004; Niedermaier, Bohrer et al 2004; Suh, Kim et al 2005; Mitchell, Teri et al 2008; Hadidi, N., Treat-Jacobson, D.J., & Lindquist, R. 2009; De Man‐van Ginkel, Gooskens et al 2010; Srivastava, Taly et al 2010; Cameron, Cheung et al 2011; Herrmann, Seitz, et al 2011; Schmid, Kroenke et al 2011; Salter, McClure et al 2012; de Man-van Ginkel, Hafsteinsdóttir et al 2013; Broomfield, Quinn, et al 2014; Mitchell, Sheth et al 2017; Sarfo, Jenkins et al 2017; Towfighi, Ovbiagele et al 2017; Das & Rajanikant 2018). Life without hope is not life at all. If post-stroke provision is poor, it is easy to lose hope because, the little support given, gradually starts to fade away, the individual is left alone, waiting for something of significance to occur, and constantly experiencing setbacks that only lead to further periods of waiting. I am currently waiting for an alternative to my catheter (waiting three months already) with which I have an ongoing problem, waiting for an electric wheelchair assessment (waiting over a month so far and almost a year post-stroke), and waiting for my virus inoculation (why, when all my able-bodied friends have been inoculated already, am I still waiting?). If the wheelchair assessment finds me competent, I, no doubt, will have another long wait to learn, and to get, what I am entitled. Do I want special treatment? No. Am I deserving of more attention because of my stroke? No, I realise I am not special but I would like just a little more understanding of my predicament. Having no electric wheelchair virtually ensures that, without the help of others, I must spend day after day in the same position, in the same bed, in the same room. Others come to see me and typically talk of the weather outside, such conversations only serving to reinforce my feeling of being shackled, unable to escape. Not that I complain about the topic of conversation, I do not want to risk visitors electing to refrain from communication with me. I am still able to laugh at my situation and the events that happen. If I could not, I think that I would go quite mad! C’est la vie, n’est-ce pas? When I feel low, I try to take my mind to a different place. I might start writing a little more of this paper, for example!
Update (some weeks later than the above paragraph):- I now have had my virus inoculations, my catheter assessment (I still need a catheter. I was in terrible pain all the time that I was without a catheter and it had to be replaced.), and the first part of an electric wheelchair assessment (I will be provided with one for which I am really grateful). I now await the second part of the assessment (an outdoor road safety assessment) that I can request when I feel confident in the wheelchair's use. Why wasn't all of this explained to me much earlier after the stroke? It would have improved the quality of my existence in the early months post-stroke when my depression was at its most intense. The requirement for better post-stroke provision is becoming clear to me. I hope that this paper will help to make it clear to others (specifically, those in a position to make things happen) too.
Update (some weeks later than the above paragraph):- I now have had my virus inoculations, my catheter assessment (I still need a catheter. I was in terrible pain all the time that I was without a catheter and it had to be replaced.), and the first part of an electric wheelchair assessment (I will be provided with one for which I am really grateful). I now await the second part of the assessment (an outdoor road safety assessment) that I can request when I feel confident in the wheelchair's use. Why wasn't all of this explained to me much earlier after the stroke? It would have improved the quality of my existence in the early months post-stroke when my depression was at its most intense. The requirement for better post-stroke provision is becoming clear to me. I hope that this paper will help to make it clear to others (specifically, those in a position to make things happen) too.
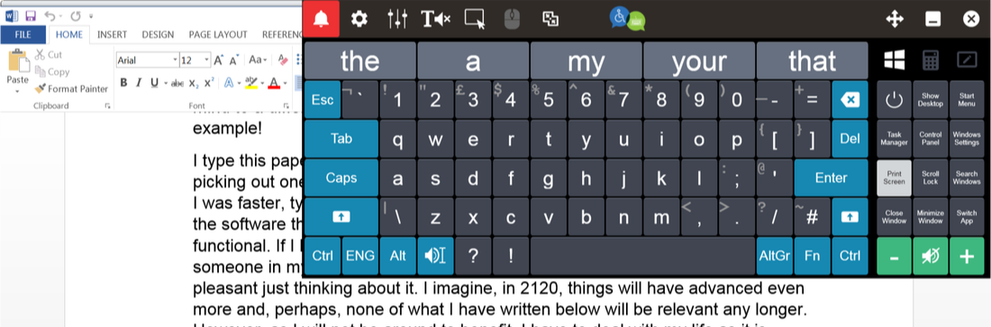
I type this paper using an on-screen keyboard called Click2Speak (it is very good and it is free)(illustrated below) and, currently, I am using an on-screen keyboard I built myself using The Grid 3 software from SmartBox (which is fantastic), controlled via a wireless trackball, picking out one letter at a time. Click2Speak was not as fast as I would have liked and it didn't have many of the features that I wanted. Having said that, Click2Speak is still very, very good. The Grid 3, however, in my opinion, is the best on-screen keyboard software currently available but it is not free (although, I think that it is worth every penny). Prior to the stroke, I was faster, typing with two able hands. I am grateful for both the technology and the software that enables me to type, while in bed, with half of my body not functional. If I have to be disabled, I am glad it is in 2020 and not in 1920! Life, for someone in my position, must have been terribly difficult a century ago. It is not pleasant just thinking about it. I imagine, in 2120, things will have advanced even more and, perhaps, none of what I have written below will be relevant any longer. However, as I will not be around to benefit, I have to deal with my life as it is today. ‘Helper robots’, programmed to meet my every need, only exist in fiction. Until they become reality, people must fulfil that function for, at least, a small part of my day. During the night, my wife was, and still is, ‘on call’ to provide my care, even at three in the morning, although she has to work during the daylight hours and needs to sleep well to be able to function. When she had a daytime job (she was a teacher), I would lay in my bed, often in some pain, during the night, trying not to call her, so as not to disturb her sleep to come and help me. However, after a while, sometimes, I could not stand being in pain any longer and simply had to wake her. This remains the situation today and I do not see it changing significantly in the near future. I have a button, by my bed, downstairs that rings a bell upstairs in the bedroom. One particularly bad night, I had to summon her three times. I feel awful doing it once during the night; imagine how I felt having to do it three times. Typically, each ‘call’ keeps my wife fully occupied for around thirty minutes and so, she loses approximately forty minutes of sleep each time I have to awaken her. I am usually awake throughout the night. My doctor prescribed medication to help me sleep but it did not work. Apparently, a doctor may not prescribe anything stronger or more effective. Such a thing must exist because they put Patients to sleep in seconds to perform surgery. As I do not sleep at night, I tend to fall asleep during the day for short ‘naps’ of perhaps an hour or two. I have fallen asleep while holding a drink in my good hand with obvious consequences! A very wet bed and more work for those having to care for me. I try not to sleep at all during the day such that I have a better chance of sleeping at night. However, my body has a will of its own and it is often stronger than my will to remain awake.

The experience I had in hospital after my stroke was not a good one overall. I scribbled notes in a jotter, throughout my stay, in rather poor quality handwriting; it is hard to write with just one hand while lying in bed with a notebook resting on the blanket, perched precariously on my remaining good raised knee. In reviewing my notes, on one page I had written, ‘I hate it here’ and on another, ‘some nurses nice, some nurses mean’. I particularly found some of the night staff I encountered to be ‘mean’. It seemed like they resented having to help me. Perhaps, having to work throughout the night is a chore and staff resent it. I can empathise with that but it is no reason to treat Patients any differently. I grew accustomed to long waits of fifteen minutes or more after pressing the nurse call button. I am aware that nursing is a busy and demanding occupation. I have nothing but respect for the job that nurses do and believe they deserve a significant pay rise to reward their dedication. However, a few are not deserving of such recognition. One night, after waiting for nearly twenty minutes for someone to answer my call, a nurse finally came to my bedside, she switched off the call light, which was flashing on the wall by my bed, and then walked away without saying or doing anything at all to or for me. My wife wrote to the Patient Experience Team to raise this issue but things did not improve. Another time, I was in a bed with a faulty bed control. It was night and the lights were out. I was very uncomfortable but could do nothing to help myself except to try to use the bed control to reposition my body a little. In the poor light, I hit the ‘raise bed’ function thinking that I was raising the top of the bed just to sit up. When I realised that I had raised the whole bed by mistake. I tried to lower it but that particular function was faulty and not working on my control, so the bed remained raised in its highest position. A while later, a night duty nurse, on seeing my elevated position, came up to me and started to scold me like a little child. I tried to explain but my speech was bad following the stroke and I struggled to speak. The nurse made no effort to listen and comprehend my poor communication and continued to berate me. He used the separate bed control at the foot of the bed to lower the bed. He told me that I should go to sleep and stop messing with the bed control as it was not safe to be
“way up in the air.”
He then took my bed control and positioned it behind me such that I could not reach it and had to spend the remaining part of the night without any control over my position whatsoever. He said that he would be in trouble if I were to fall out of bed so high up (where was the concern for me?). Fall out? I could not even roll over on my own let alone fall out of bed. The side railings were in use and in the up position! How could I possibly fall out of bed even if the bed was atop a mountain? That particular nurse showed no understanding of my condition or my predicament. I was just a ‘naughty child’ messing with the bed control in his mind. On yet another night, I had been moved from the main stroke ward to an individual room, for a reason that I do not remember, and I really was really in need of a drink. I was so dry. I pressed the nurse call button and waited. Twenty minutes later (I got into the habit of timing my ‘waits’), I heard nurses talking outside my room;
“Who’s buzzing?” “Oh, it’s just the man in room x. He can wait.”
I waited another fifteen minutes before I got a drink. It got so that I dreaded the night. I was not sleeping well and would lie awake becoming more uncomfortable because I was unable to adjust my position sufficiently. It is unnatural to remain in the same position for long in bed, recordings of sleep patterns show regular body movement throughout the night (https://www.23andme.com/en-gb/topics/wellness/sleep-movement/). I lay awake for hours, much of the time, trying to move my body a little, using a combination of the bed control and my one good leg, to make myself more comfortable and ease the increasing pain, particularly in my bottom. I lay, waiting for the daybreak when, just before breakfast, nurses would arrive to wash me and make me comfortable, ready for the day to come. Time passes slowly when there is little to do to occupy the mind. I was very reluctant to use the nurse call button because my previous experiences were less than positive. I would lie, in some degree of discomfort, longing for someone who would come and help me. Some nurses were fantastic and nothing seemed too much trouble for them. One nurse sat by my bedside one day when I was feeling particularly low. She took the time to talk to me and tell me of other people she had met who had a stroke like mine and made an amazing recovery. She even held my hand. She was positive and caring. I wish all nurses were like her.
“way up in the air.”
He then took my bed control and positioned it behind me such that I could not reach it and had to spend the remaining part of the night without any control over my position whatsoever. He said that he would be in trouble if I were to fall out of bed so high up (where was the concern for me?). Fall out? I could not even roll over on my own let alone fall out of bed. The side railings were in use and in the up position! How could I possibly fall out of bed even if the bed was atop a mountain? That particular nurse showed no understanding of my condition or my predicament. I was just a ‘naughty child’ messing with the bed control in his mind. On yet another night, I had been moved from the main stroke ward to an individual room, for a reason that I do not remember, and I really was really in need of a drink. I was so dry. I pressed the nurse call button and waited. Twenty minutes later (I got into the habit of timing my ‘waits’), I heard nurses talking outside my room;
“Who’s buzzing?” “Oh, it’s just the man in room x. He can wait.”
I waited another fifteen minutes before I got a drink. It got so that I dreaded the night. I was not sleeping well and would lie awake becoming more uncomfortable because I was unable to adjust my position sufficiently. It is unnatural to remain in the same position for long in bed, recordings of sleep patterns show regular body movement throughout the night (https://www.23andme.com/en-gb/topics/wellness/sleep-movement/). I lay awake for hours, much of the time, trying to move my body a little, using a combination of the bed control and my one good leg, to make myself more comfortable and ease the increasing pain, particularly in my bottom. I lay, waiting for the daybreak when, just before breakfast, nurses would arrive to wash me and make me comfortable, ready for the day to come. Time passes slowly when there is little to do to occupy the mind. I was very reluctant to use the nurse call button because my previous experiences were less than positive. I would lie, in some degree of discomfort, longing for someone who would come and help me. Some nurses were fantastic and nothing seemed too much trouble for them. One nurse sat by my bedside one day when I was feeling particularly low. She took the time to talk to me and tell me of other people she had met who had a stroke like mine and made an amazing recovery. She even held my hand. She was positive and caring. I wish all nurses were like her.
I started to believe that hospital is the worst place to be when ill. My hospital was charging £10 per day just to watch TV. I refused to pay such an exorbitant amount and, as listening to the radio was free (when it was working), I would do that instead. My wife came to see me every day. How I looked forward to her visits. I asked her to buy me a DVD player and to scour the local charity shops and purchase any films on disc she found that she thought I might like. Doing all of that was much less expensive than paying for the ‘privilege’ of watching hospital TV. I passed the long days and nights watching film after film, even though I had seen most of the films before. I longed to go home from hospital so that I could recover. It would be weeks before my wish came true and then a completely new set of issues with post-hospital provision and care teams would arise. Do staff receive training in basic Patient / Client care? If they do, some attending must be sleeping throughout the course or the course is not fit for purpose. My experiences prompted me to write this paper to give those in a caring or administrative role a basic guide to good practice written by someone with first hand and current experience of care / Patient provision; an insider’s view.
I wish to make it clear that, although this page may read like a criticism of Carers and Nurses, it would be mistaken to conclude I have a negative opinion of people working as either Carers or Nurses. Far from it! I have encountered many outstanding Carers and Nurses. I believe both deserve a higher status for the essential function they play in society. Where would I be without them? In a very bad situation without doubt. However, no matter how good a Carer/Nurse is, there is always some room for improvement. Client feedback is therefore important (Tasa, Baker, & Murray 1996; Vingerhoets, & Grol 2003; Bastemeijer, Boosman et al 2019; Berger, Saut, & Berssaneti 2020). As feedback, I hope this paper helps.
Below are sixty something points I have noted/experienced as an IRON POD confined mostly to bed and with knowledge gained through my earlier work (as a TAB – Temporarily Able Bodied person) in supporting special needs across the world over many years. The points made are grouped together under subheading categories. These are not in any particular order of importance. Some points deal specifically with my time spent in hospital and relate to the nursing provision. Others relate specifically to post-hospital care provided at home. Most are equally relevant to both forms of provision. I use the term ‘Client’ throughout this text to refer to the person in need of assistance. A ‘Client’ may be called a service user, a customer, a Patient, or some other term of reference, depending upon your specific area of provision. ‘Carer’ is used throughout to denote the provider of care be it a qualified nurse or a person working in a caring role for a care provision company. I use the term ‘Patient’ if the experience directly relates to my time in hospital although the point made might equally relate to both areas of provision. 'Significant Other' is used to describe any person identified as significant who interacts with and / or enables a Client. This will include a spouse, partner or other family member, friend, and any person who is likely to have more than a passing interest in the Client and with whom the Client may attempt to communicate, in any way, on a reasonably frequent basis.The acronym POD is used to represent a Person Of Disability or People Of Disability depending on context. The acronym IRON is also used frequently throughout this page. Its meaning was detailed earlier on this page.
This page is divided into seven sections, each dealing with a specific aspect of my new experience as an IRON POD.
a) The goal is Control (Follows immediately)
b) Communication (Starts just after point 8)
c) Client Care and Care Practice (Starts just before point 17)
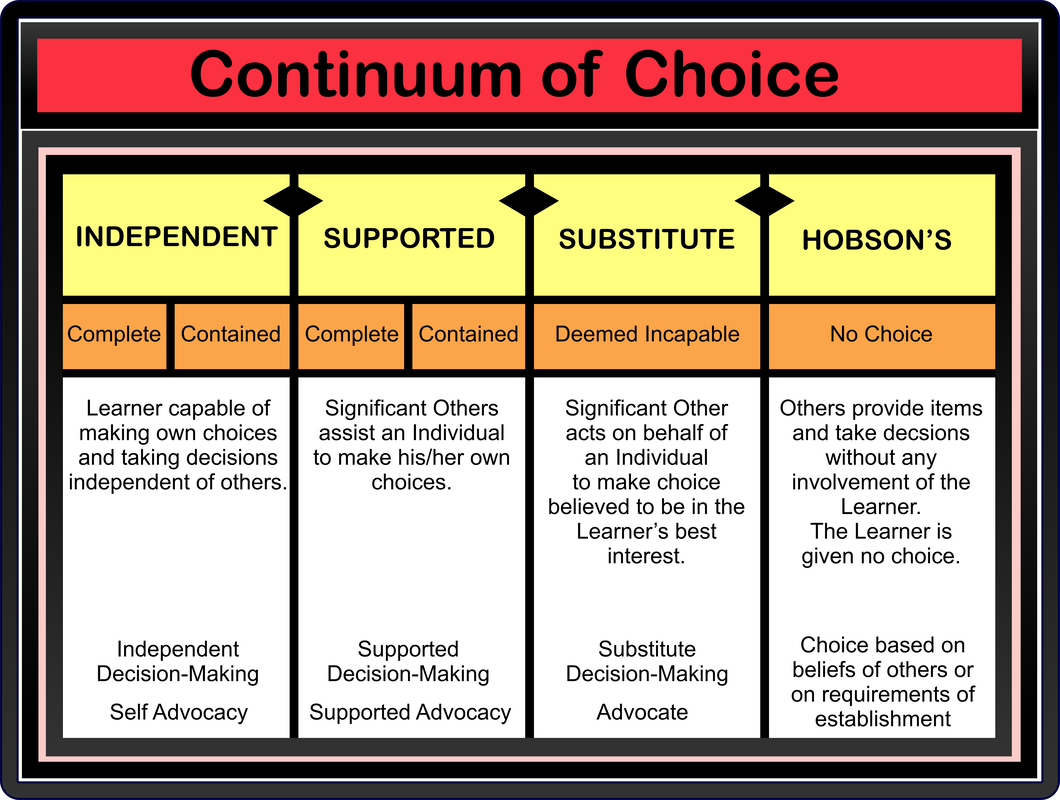
d) Choice is a Voice (Starts just before point 56)
e) Eating and Drinking (Starts just before point 59)
f) Consultation and Coordination (Post-Stroke Provision) (Starts just before point 61)
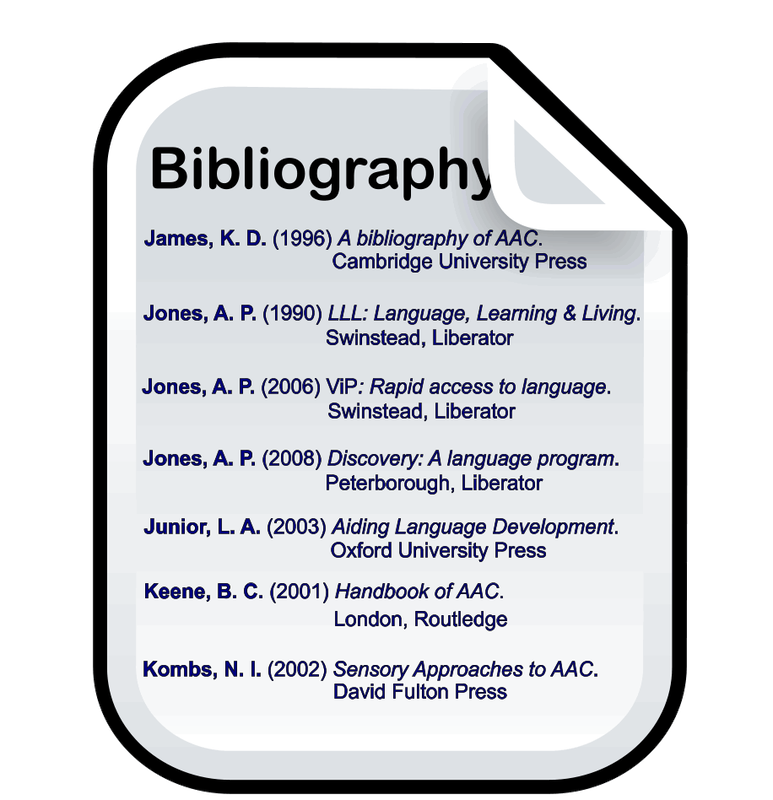
g) Bibliography and References (Starts after point 65)
The first of these is: -
This page is divided into seven sections, each dealing with a specific aspect of my new experience as an IRON POD.
a) The goal is Control (Follows immediately)
b) Communication (Starts just after point 8)
c) Client Care and Care Practice (Starts just before point 17)
d) Choice is a Voice (Starts just before point 56)
e) Eating and Drinking (Starts just before point 59)
f) Consultation and Coordination (Post-Stroke Provision) (Starts just before point 61)
g) Bibliography and References (Starts after point 65)
The first of these is: -
The Goal Is Control / Control is the Goal.
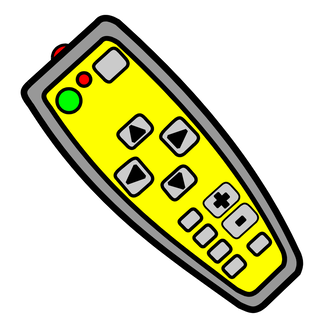
1. The goal is control. That means giving the Client control and not taking it away from him or her. If remote controls are in use, the Carer should not take control but pass the control of the situation to the Client (Barlow, Wright et al 2002; Greene & Hibbard 2012 ; Foot, Gilburt et al 2014; McDonald C., 2014). If the person is not capable of operating the control, you should always ask for permission to use it and state clearly what you are about to do. Ask permission before each action:
“Is it OK if I lower your head?"
"Is it okay for me to mute the sound on the TV?"
Even if the person is physically incapable of performing some function, ensure that the person is always in control. Never take the bed control without permission and subsequently ask,
“Is it alright to raise the bed?”
The former act negates the latter. When a Carer takes control by removing Client control, this also removes Client dignity. Ensure the Client remains in full control when s/he is alone. Do they have the TV remote? Is the bed control accessible? Is the call button available? I found myself, on numerous occasions, without a means of summoning assistance. It is very worrying, especially if you are in a room on your own. I soon learned to check that I had access to a call button before staff left and I was on my own. That situation is not as threatening for more able Clients (who are not helpless and can get out of bed and move around to do things for themselves), but I was an IRON POD, a prisoner within my bed, held captive by my disability. I was not in control. Early in my first period in hospital following the stroke, I had to call a nurse to look at my catheter bag, which was full. The nurse said,
“Oh Christ!”
and hurried to get a disposable bottle in which to empty it. I then asked the nurse for the bed control. She gave me a quizzical look and asked,
“What do you want that for?”
I explained that I wanted to raise the top of the bed. She asked,
“Do you want to sit up?”
and using the bed control herself proceeded to raise the top of the bed saying,
“Tell me when.”
I protested,
“No, give the control to me.”
My speech was poor, affected by the stroke, and the nurse just carried on in control saying,
“Too high?”
and began lowering the top of the bed! I repeated, as clearly as I was able,
“No, give it to me.”
This time the nurse appeared to understand me and passed me the control stating,
“Fine, do it yourself.”
She was not pleased as she walked away. Carers like to be in control. It is not the Carer that needs to be in control, it is the Client. An example will illustrate this concept further. I had been saving some dental chewing gum on a little piece of tin foil on my bed table. I had a piece of gum every day and I had saved it over a week. It may not have been too hygienic but it was my choice. One morning a Carer spotted the gum on my table and, without asking me, picked it up and threw it in the rubbish bag! I was angry that she had taken away my control. The goal is control. Control over health. Control over Carers. Control over the environment. Control over the gadgets in the environment. Control over my own being. Control is empowering.
Update October 2021 I had to return to King's Mill Hospital after contracting a serious infection. The standard of care showed no improvement. At lunchtime on Monday 25th October a lady (I don't think that she was a nurse)brought me my dinner and told me to sit myself up for my meal. I reached for the bed control handset to sit myself up carefully. I was not in a good position in bed and raising the top part of the bed would bend me awkwardly and cause me a lot of pain if taken too far without care. Because of my disability, I cannot do things as fast as I used to do and the lady started to raise the top using the control at the bottom of the bed, taking control without asking me. I immediately told her to stop. She replied angrily, informing me patronisingly that I had to sit up to eat or I could choke. I informed her that I was an adult, not a child, and I could raise the top of my bed myself. At which point, she turned away and walked out of my room. To cap it all, when I tried the dinner it was barely warm. I didn’t eat it.
On Monday afternoon, my wife brought me a portable DVD player and some DVDs to watch as there is nothing to do in a single room in hospital. There was a television but they were charging £10 a day for the privilege of watching it. I barely watch TV at home, I wasn’t going to pay ten pounds every day to watch what I would consider poor quality programmes. The DVD player had a sprung top which, when opened, formed the screen. That evening I decided to watch a film and tried to open the lid on the player such that I could insert the DVD and play the movie. Opening a sprung lid with just one functioning hand is really difficult. I spent half an hour trying to balance the player on my legs, while in bed (not sitting up fully), at the same time, endeavouring to open a lid that was fighting to remain closed. At 21:30, I gave up my attempt and decided that I required some assistance. I pressed the nurse call button. Fifteen minutes later, I was thirsty so I reached for my drink and took a few sips. Attached to my cannula was a tube running down from a saline bag. The tube ran through a very annoying device that regulated and monitored the flow. Annoying because it would emit a continuous series of loud beeps when it encountered any issue and I had no means of stopping the beeps myself without summoning a nurse. Raising my good arm to take a drink, set the device off and I was subjected to continuing loud beeping. Why the nurses didn’t put the cannula in my paralysed arm which, obviously, didn’t move, I will never know. Putting it in my functional arm meant that I could not raise it to have a drink or adjust my glasses or scratch my nose without setting off that darn alarm. I had called for a nurse at 21:30, the drip feed alarm went off at 21:45, but help did not arrive until 22:15, some 45 minutes after I had called for help. If I had been in serious trouble, I could have died before anyone answered my call for help. I timed every response while in hospital. A habit I developed during my previous stays there following my stroke a year before. The average time it took a nurse to respond to the nurse call button was 15 minutes! 45 minutes was even worse. The nurse that came was called Alice. I told her my tale and she apologised profusely. Alice explained that she had been on the medication round and was therefore busy with other duties. I expressed concern that there should be other nurses available to answer calls for help. Alice said that there was one other nurse on duty but didn’t know what she was doing or why she hadn’t responded. Alice was very good and very caring and very helpful, I took an instant liking to her. I don’t have a negative word to say about her. However, 45 minutes to respond to what, potentially, may have been a serious distress call is appalling and unacceptable in any hospital, let alone one that proudly displays an ‘outstanding’ award for care from the CQC inspectorate in its entrance hall.
On the following day, nurses came to adjust my position and make me comfortable but left me quickly to attend to another matter. However, they left me without:
• access to my nurse call button;
• access to the bed control handset;
• a bedside table which they had moved in order to help me but not replaced;
• access to a drink. My drinks were on my bed table which was moved;
• access to entertainment (also on my bed table).
I was completely helpless. I could not call for help, I could not reach my nurse call button. I could not even adjust my position. I simply had to wait until someone happened to walk into my room. I could have been stranded for hours before that happened but, as luck would have it, my wife walked in a few minutes later on her daily visit. The whole situation was a further example of the quality of the care practice in the hospital. Surely, it just couldn't be happening to me?
“Is it OK if I lower your head?"
"Is it okay for me to mute the sound on the TV?"
Even if the person is physically incapable of performing some function, ensure that the person is always in control. Never take the bed control without permission and subsequently ask,
“Is it alright to raise the bed?”
The former act negates the latter. When a Carer takes control by removing Client control, this also removes Client dignity. Ensure the Client remains in full control when s/he is alone. Do they have the TV remote? Is the bed control accessible? Is the call button available? I found myself, on numerous occasions, without a means of summoning assistance. It is very worrying, especially if you are in a room on your own. I soon learned to check that I had access to a call button before staff left and I was on my own. That situation is not as threatening for more able Clients (who are not helpless and can get out of bed and move around to do things for themselves), but I was an IRON POD, a prisoner within my bed, held captive by my disability. I was not in control. Early in my first period in hospital following the stroke, I had to call a nurse to look at my catheter bag, which was full. The nurse said,
“Oh Christ!”
and hurried to get a disposable bottle in which to empty it. I then asked the nurse for the bed control. She gave me a quizzical look and asked,
“What do you want that for?”
I explained that I wanted to raise the top of the bed. She asked,
“Do you want to sit up?”
and using the bed control herself proceeded to raise the top of the bed saying,
“Tell me when.”
I protested,
“No, give the control to me.”
My speech was poor, affected by the stroke, and the nurse just carried on in control saying,
“Too high?”
and began lowering the top of the bed! I repeated, as clearly as I was able,
“No, give it to me.”
This time the nurse appeared to understand me and passed me the control stating,
“Fine, do it yourself.”
She was not pleased as she walked away. Carers like to be in control. It is not the Carer that needs to be in control, it is the Client. An example will illustrate this concept further. I had been saving some dental chewing gum on a little piece of tin foil on my bed table. I had a piece of gum every day and I had saved it over a week. It may not have been too hygienic but it was my choice. One morning a Carer spotted the gum on my table and, without asking me, picked it up and threw it in the rubbish bag! I was angry that she had taken away my control. The goal is control. Control over health. Control over Carers. Control over the environment. Control over the gadgets in the environment. Control over my own being. Control is empowering.
Update October 2021 I had to return to King's Mill Hospital after contracting a serious infection. The standard of care showed no improvement. At lunchtime on Monday 25th October a lady (I don't think that she was a nurse)brought me my dinner and told me to sit myself up for my meal. I reached for the bed control handset to sit myself up carefully. I was not in a good position in bed and raising the top part of the bed would bend me awkwardly and cause me a lot of pain if taken too far without care. Because of my disability, I cannot do things as fast as I used to do and the lady started to raise the top using the control at the bottom of the bed, taking control without asking me. I immediately told her to stop. She replied angrily, informing me patronisingly that I had to sit up to eat or I could choke. I informed her that I was an adult, not a child, and I could raise the top of my bed myself. At which point, she turned away and walked out of my room. To cap it all, when I tried the dinner it was barely warm. I didn’t eat it.
On Monday afternoon, my wife brought me a portable DVD player and some DVDs to watch as there is nothing to do in a single room in hospital. There was a television but they were charging £10 a day for the privilege of watching it. I barely watch TV at home, I wasn’t going to pay ten pounds every day to watch what I would consider poor quality programmes. The DVD player had a sprung top which, when opened, formed the screen. That evening I decided to watch a film and tried to open the lid on the player such that I could insert the DVD and play the movie. Opening a sprung lid with just one functioning hand is really difficult. I spent half an hour trying to balance the player on my legs, while in bed (not sitting up fully), at the same time, endeavouring to open a lid that was fighting to remain closed. At 21:30, I gave up my attempt and decided that I required some assistance. I pressed the nurse call button. Fifteen minutes later, I was thirsty so I reached for my drink and took a few sips. Attached to my cannula was a tube running down from a saline bag. The tube ran through a very annoying device that regulated and monitored the flow. Annoying because it would emit a continuous series of loud beeps when it encountered any issue and I had no means of stopping the beeps myself without summoning a nurse. Raising my good arm to take a drink, set the device off and I was subjected to continuing loud beeping. Why the nurses didn’t put the cannula in my paralysed arm which, obviously, didn’t move, I will never know. Putting it in my functional arm meant that I could not raise it to have a drink or adjust my glasses or scratch my nose without setting off that darn alarm. I had called for a nurse at 21:30, the drip feed alarm went off at 21:45, but help did not arrive until 22:15, some 45 minutes after I had called for help. If I had been in serious trouble, I could have died before anyone answered my call for help. I timed every response while in hospital. A habit I developed during my previous stays there following my stroke a year before. The average time it took a nurse to respond to the nurse call button was 15 minutes! 45 minutes was even worse. The nurse that came was called Alice. I told her my tale and she apologised profusely. Alice explained that she had been on the medication round and was therefore busy with other duties. I expressed concern that there should be other nurses available to answer calls for help. Alice said that there was one other nurse on duty but didn’t know what she was doing or why she hadn’t responded. Alice was very good and very caring and very helpful, I took an instant liking to her. I don’t have a negative word to say about her. However, 45 minutes to respond to what, potentially, may have been a serious distress call is appalling and unacceptable in any hospital, let alone one that proudly displays an ‘outstanding’ award for care from the CQC inspectorate in its entrance hall.
On the following day, nurses came to adjust my position and make me comfortable but left me quickly to attend to another matter. However, they left me without:
• access to my nurse call button;
• access to the bed control handset;
• a bedside table which they had moved in order to help me but not replaced;
• access to a drink. My drinks were on my bed table which was moved;
• access to entertainment (also on my bed table).
I was completely helpless. I could not call for help, I could not reach my nurse call button. I could not even adjust my position. I simply had to wait until someone happened to walk into my room. I could have been stranded for hours before that happened but, as luck would have it, my wife walked in a few minutes later on her daily visit. The whole situation was a further example of the quality of the care practice in the hospital. Surely, it just couldn't be happening to me?
2. Stop banging. One time, while in hospital, I found myself with no access to a nurse call button. I could not shout,as a result of the stroke I could hardly speak and, when I did manage to speak, it was barely intelligible. Needing assistance, I improvised and used the bed control pendant to bang on the bed frame. The unorthodox technique worked in that it got attention but I was scolded (banging was ‘inconsiderate of other patients’) and I had the bed control taken away and moved out of my reach! However, the nurse did give me the nurse call button but it was at the cost of losing my bed control. Ensure the Client always has an acceptable means of summoning assistance. Never punish a Client by removing control. The removal of a Patient's control is the removal of a Patient's dignity.
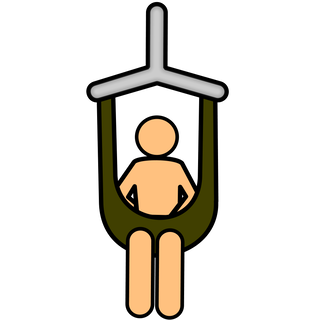
3. Going up? Ensure the hoist is in good working order (Health and Safety Executive 2011; Bainbridge 2019). If the Client is capable, put control of the hoist in the Client’s hands. Give control of the hoist to the person to be hoisted. The Carers can ensure that hoisting is undertaken safely even when they are not directly holding the hoist control. If the individual is physically and cognitively competent, the role of the Carer is to empower the Client and enable him / her to do it for him / herself. If there is no other option but for Carers to operate the hoist, it is important that they allow the Client to take charge of the situation by asking the person to give instructions on what actions to take and when to take them. Client instructions need not be verbal, sign or gesture are equally as good; these modes of communication still allow the Client control of the situation. Do not take control away from the Client, allow the Client gradually to take control away from you. The goal is control. Client control.
4. I’m in charge. Who is in charge? (Haug & Lavin 1981; Veatch 2008) A Carer entered my room while I was watching a film. She took the TV remote off my bed and paused the film without asking. I was somewhat annoyed! Her actions implied that she was in charge of the situation and, now that she was present, I was subject to her will. The question of who is in ultimate control of a situation can be contentious. If a Client is saying one thing and the Client’s spouse (or Significant Other) another and the Carer’s belief is yet a further option, whose rule is correct? Sometimes this can be problematic. As a general principle, the Client should always have the guiding voice, although it may prove very difficult to ignore the spouse! Suppose the Client is not cognitively competent, should the spouse’s wishes prevail? The answer is not a simple ‘yes’. The Client’s wishes should always be a priority but an other’s wishes may overrule a Client if the Client’s wish is D.U.B.I.O.U.S:
- Dangerous,
- Unreasonable (impartial others would judge it to be so),
- Bad (for the Client), (who decides what is bad for the Client?!)
- Impossible to undertake,
- Outside your remit, (there may be rules that do not permit Carers to perform specific actions. This includes any directive written into the Client’s Care Plan),
- Unintelligible or Unworkable,
- Specialist (requires a professional – a person specifically qualified for that role)
5. Empathy. Anyone’s life can change, in an instant, overnight. It could be you lying naked in the bed unable to care for yourself, unable to move without assistance. How would you feel? How would you want to be treated? (Raab 2014; Svenaeus 2015). While there would be gratitude to those who gave up their time to come and do anything just to be of help (family, friends, old colleagues, volunteers) there would be a far greater expectation of others who were being paid to provide assistance, especially if it were your money that was used. If you were paying, would you expect a basic standard of service? Would you be concerned about the issues raised on this page? Imagine being naked while other virtual strangers were touching intimate parts of your anatomy. That is what will happen if you become an IRON POD club member. It is a club that anyone can join: male or female, rich or poor, black or white, old or young. It is a club to which no person chooses to belong. Why? Because the rules are so harsh. The first rule of the IRON POD club is members don't elect to join the club, the club elects to join a member. A person has only a limited ability in preventing membership. That is because most people believe that it will never happen to them. The annual membership fee is very large and, once a member, it is almost impossible to leave.

6. Mrs Stretch and Mr Bendy. Unless very special, a person’s elbows only bend in one direction. Why, then, do some Carers place items, such as the bed control, TV remote, etc., in positions that require the Client to perform superhuman contortions in order to be able to access them? Placing items in impossible to reach locations is removing Client control. Removing control is removing dignity. Maintenance of the Client’s dignity is extremely important (Cairns, Williams et al 2013; Higgins 2020; Hammar, Alam et al 2021). The goal is control. The goal is Client control. (Examples of removal of Client dignity can be found in a Unison publication available here: https://www.unison.org.uk/content/uploads/2015/06/23070.pdf)
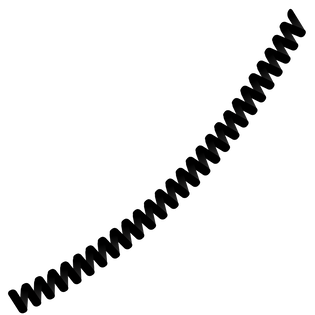
7. Enable with the cable. Controls for hospital-style beds are usually attached to the bed via a spiralling cable. This cable has a habit of becoming snagged down the side of the bed such that only a small amount is available to the Client in attempting to control the bed’s position. The Client ends up fighting against the spring of the spiral to gain control. Carers have stood and watched me struggle with the bed control, fighting against the springy cable and not asked if I needed help. When a person has only one working hand, trying to operate controls on an item attached to a spring is something of a problem! As soon as an attempt is made to press a button, the bed control flies away from the hand pulled by the spring of the cable!! It is either hold the control against the spring of the cable or operate the control itself. It is very difficult to do both at the same time with just one hand. On passing a bed control to a Client, always ensure that the cable is free.
It is a simple matter for a Carer to ensure the bed control is within reach, easily accessible, and the cable is free from snagging on the side of the bed. The Client should be able to use the control after Carers leave without any problems. I am amazed that in this day and age that there needs to be a cable at all. Why isn't the bed control remote?
I have been having care for over a year now and still the majority of Carers pass me the bed control without freeing the cable. I have to struggle with the cable until someone notices and helps.
It is a simple matter for a Carer to ensure the bed control is within reach, easily accessible, and the cable is free from snagging on the side of the bed. The Client should be able to use the control after Carers leave without any problems. I am amazed that in this day and age that there needs to be a cable at all. Why isn't the bed control remote?
I have been having care for over a year now and still the majority of Carers pass me the bed control without freeing the cable. I have to struggle with the cable until someone notices and helps.
8. Assess not Assume (Ryden & Knopman 1989). Do not assume because ass-u-me makes an ass out of u (you) and me (pun originally attributed to Oscar Wilde). Do not assume that a Client cannot comprehend questions or instructions. Do not assume that a Client is incapable of performing a task even if the Client’s ability is unclear. Rather, clarify the situation by asking the person. Never perform an action on ‘behalf of an individual’ assuming the person cannot do it for him / herself. Take away a Client’s control and take away a Client’s dignity. Under time constrictions, it is often easier / quicker to ‘do for’. This is not good practice.
Do for = poor practice.
Do with = better practice.
Enabling the Client to do for him / herself = best practice.
Do for = poor practice.
Do with = better practice.
Enabling the Client to do for him / herself = best practice.
Communication
 V-Pen System
V-Pen System
Communication is important.
Speech is power in our society. Hence, it should surprise no one that freedom of speech is the first right guaranteed to all Americans in the Bill of Rights. Deprived of speech or another means of effective communication, individuals become invisible. They are simply not heard. They are silenced. And, when people are silenced, others quickly lose sight of their right to be a part of humanity! (Bryen D. 1993)
The limits of my language mean the limits of my world (Wittgenstein L. 1953)
No one in this day and age can possibly underestimate the importance of language. We are surrounded by talking (Jeffree D. & McConkey R. 1976)
Speech is the most important thing we have. It makes us a person and not a thing. No one should ever have to be a 'thing.' (Joseph D. 1986)
The ability to communicate, that is, to interact socially and to make needs and wants known, is central to the determination of an individual’s quality of life. The power of communication is especially important for the severely handicapped .... these individuals face a lifetime of substantial, if not total dependence on others; hence, their ability to communicate and establish some control over their environment must be recognized as a priority in their programming (Light J., McNaughton D., & Parnes P. 1986)
And to be defective in language, for a human being, is one of the most desperate of calamities, for it is only through language that we enter fully into our human estate and culture, communicate freely with our fellows, acquire and share information. If we cannot do this, we will be bizarrely disabled and cut off - whatever our desires, or endeavours, or native capacities. And indeed, we may be so little able to realize our intellectual capacities as to appear mentally defective. (Sacks O. 1989)
My basic problem was one I’ve encountered through my whole life. When you can’t talk, and people believe that your mind is as handicapped as your body, it’s awfully difficult to change their opinion. (Sienkiewicz‑Mercer R. & Kaplan S. B. 1989)
A communication handicap is quite different from other handicaps. It affects the manner in which you relate to other people and how they relate to you, it pervades everything you do (Oakley M. 1991)
Imagine a life without words! Trappist monks opt for it. But most of us would not give up words for anything. Every day we utter thousands and thousands of words. Communicating our joys, fears, opinions, fantasies, wishes, requests, demands, feelings - and the occasional threat or insult - is a very important aspect of being human. The air is always thick with our verbal emissions. There are so many things we want to tell the world. Some of them are important, some of them are not. But we talk anyway - even when we know that what we are saying is totally unimportant. We love chitchat and find silent encounters awkward, or even oppressive. A life without words would be a horrendous privation. (Katamba F. 1994)
Language is so tightly woven into human experience that it is scarcely possible to imagine life without it. Chances are that if you find two or more people together anywhere on earth, they will soon be exchanging words. When there is no on to talk with, people talk to themselves, to their dogs, even to their plants. In our social relations, the race is not to the swift but to the verbal - the spellbinding orator, the silver-tongued seducer, the persuasive child who wins the battle of wits against a brawnier parent. Aphasia, the loss of language following brain injury, is devastating, and in severe cases family members may feel that the whole person is lost forever. (Pinker S. 1994)
People with communications deficits face particular challenges unique to them. It is through communicative interactions that individuals are able to transcend the barriers erected by disability. Being unable to speak creates special problems. A well-used communication aid can be an effective tool for integrating people with communication disabilities into the culture of a particular workplace. (Dickerson L. 1995)
And language remains our greatest treasure, for without it we are confined to a world that, while not one of social isolation, is surely one that is a great deal less rich. Language makes us members of a community, providing us with the opportunity to share knowledge and experiences in a way no other species can. (Dunbar R. 1996)
Communication is the basis of learning. Communication is essential for the acquisition of knowledge. How are we to tell whether an individual (with severe physical impairment) has internalised language unless s/he can communicate? It is imperative that the neurological development of language skills are given every opportunity to proceed without impediment (Jones A.P. 1996)
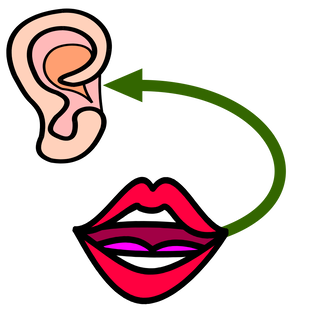
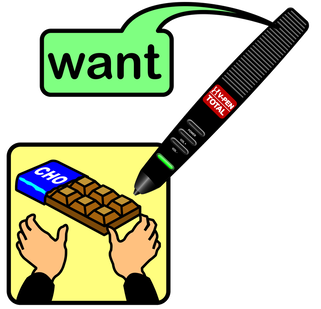
A stroke can take away the power of speech. My stroke left me with very poor speech. On good days I can make myself understood but on bad days I have no speech at all. I have worked with AAC (Alternative and Augmentative Communication) throughout my working life. I have taught AAC, designed and developed AAC, marketed AAC, and lectured on AAC all over the world. After the stroke I became a consumer of AAC. I am probably the only person in the world to have occupied each of those roles. The irony of becoming a user of AAC is not lost on me. While in hospital I used a combination of very poor natural speech, my V-Pen and board, Makaton signing, and writing in a notebook at various times in order to communicate and get what I needed to say across to others. Makaton signing is tailored for use with two able hands, I only had one functioning upper limb following the stroke and even that was not very able. I had to use Makaton creatively, adapting signs made using two hands into a single handed form. It would not have mattered if I had the use of my left hand however because none of my nurses knew any Makaton. I had to teach them some signs by signing a single word and then writing down its meaning in my notebook. A very slow way to communicate! I also used my V-Pen and board. The V-Pen is a clever pen-shaped device that can recognise symbols and speak their meaning when a symbol is touched. I was involved in the system's development when I worked for Unlimiter in Taipei, Taiwan. The nurses were more interested in the Pen, it's technology, and how it worked than what I was trying to say. Many times I forgot my intended message because I became distracted in performing to an audience of nurses showing them the Pen! I had built several communication boards for use with the Pen whilst in Taiwan which I had at home. My wife brought them for me when she came to visit. While the V-Pen was a perfect AAC system for use in hospital, unfortunately the boards that I designed were not! They did not have the vocabulary necessary for use on a hospital ward.I busied myself with the design of a board that would be highly suited for this purpose and could be available on every hospital ward throughout the world. The V-Pen system is perfect for that situation because it is small, portable, and requires virtually no learning; a person could learn to use it in seconds. The spelling board option can say virtually anything provided the Patient can spell. Put that together with a couple of symbol boards and you have a really good communication system for nurses to loan to Patients during their hospital stay.
Yes, communication matters. My lack of effective communication let me down on several occasions during my time in hospital. Some are detailed on this web page. I continue to have communication difficulties nearly a year post-stroke. I guess I will have them for the remainder of my life. Silence is not golden despite what the song says. I am already beginning to notice subtle differences in the way I am treated by others. Others are uncomfortable with silence and, as I take longer to respond to communication from other people, will 'jump in' and continue communicating in what, I presume, is an effort to ease the discomfort that I must be feeling not being able to communicate effectively.There have been other barely perceivable changes too. I will not list them here but rather attempt to cover each of them in the points that I make on the remainder of this page.
I am going to have to think about my primary mode of communication for the future if my speech continues to fail me. I have considered the development of a one-handed Makaton signing system which I have tentatively called 'Maka-One'. I have not discussed my idea with the team at Makaton yet, they may not like my idea. Presently, that is all it is, an idea. There are a few single-handed sign languages already in existence (I believe Irish Sign Language is among them) but, I would have to learn them. I already know Makaton and have started adapting it for my own personal use. I believe Beyoncé has a song about it whose lyrics are something like “All the single handers, all the single signers, if you like it then you shoulda put a patenting on it”. Well, it is something near to that, I think!! Seriously, signing with just a single available hand is no joke! Having to use my one good arm and hand for everything is putting a strain on it and I am already beginning to notice it is starting to feel uncomfortable in use and it is hurting a little to bend my fingers into a fist. This is somewhat worrying for future signing, for instance. I try to take it easier but, then, I have no hands and how do I interact with my environment? I spend a great deal of the average day completely on my own, alone in bed in a room unable to get out of bed and do any of the things I used to take for granted. I have an emergency contact button which, if I were to use it, would contact an outside service to summon help. In such a situation, my speech would certainly fail me. It is good that the line knows who and where I am and has the details of emergency contacts, even if I could not say a word during any use. The service is not free, it costs me around £20 per month. Disability doesn't come cheap in 2021. I suspect it has always been so.
Speech is power in our society. Hence, it should surprise no one that freedom of speech is the first right guaranteed to all Americans in the Bill of Rights. Deprived of speech or another means of effective communication, individuals become invisible. They are simply not heard. They are silenced. And, when people are silenced, others quickly lose sight of their right to be a part of humanity! (Bryen D. 1993)
The limits of my language mean the limits of my world (Wittgenstein L. 1953)
No one in this day and age can possibly underestimate the importance of language. We are surrounded by talking (Jeffree D. & McConkey R. 1976)
Speech is the most important thing we have. It makes us a person and not a thing. No one should ever have to be a 'thing.' (Joseph D. 1986)
The ability to communicate, that is, to interact socially and to make needs and wants known, is central to the determination of an individual’s quality of life. The power of communication is especially important for the severely handicapped .... these individuals face a lifetime of substantial, if not total dependence on others; hence, their ability to communicate and establish some control over their environment must be recognized as a priority in their programming (Light J., McNaughton D., & Parnes P. 1986)
And to be defective in language, for a human being, is one of the most desperate of calamities, for it is only through language that we enter fully into our human estate and culture, communicate freely with our fellows, acquire and share information. If we cannot do this, we will be bizarrely disabled and cut off - whatever our desires, or endeavours, or native capacities. And indeed, we may be so little able to realize our intellectual capacities as to appear mentally defective. (Sacks O. 1989)
My basic problem was one I’ve encountered through my whole life. When you can’t talk, and people believe that your mind is as handicapped as your body, it’s awfully difficult to change their opinion. (Sienkiewicz‑Mercer R. & Kaplan S. B. 1989)
A communication handicap is quite different from other handicaps. It affects the manner in which you relate to other people and how they relate to you, it pervades everything you do (Oakley M. 1991)
Imagine a life without words! Trappist monks opt for it. But most of us would not give up words for anything. Every day we utter thousands and thousands of words. Communicating our joys, fears, opinions, fantasies, wishes, requests, demands, feelings - and the occasional threat or insult - is a very important aspect of being human. The air is always thick with our verbal emissions. There are so many things we want to tell the world. Some of them are important, some of them are not. But we talk anyway - even when we know that what we are saying is totally unimportant. We love chitchat and find silent encounters awkward, or even oppressive. A life without words would be a horrendous privation. (Katamba F. 1994)
Language is so tightly woven into human experience that it is scarcely possible to imagine life without it. Chances are that if you find two or more people together anywhere on earth, they will soon be exchanging words. When there is no on to talk with, people talk to themselves, to their dogs, even to their plants. In our social relations, the race is not to the swift but to the verbal - the spellbinding orator, the silver-tongued seducer, the persuasive child who wins the battle of wits against a brawnier parent. Aphasia, the loss of language following brain injury, is devastating, and in severe cases family members may feel that the whole person is lost forever. (Pinker S. 1994)
People with communications deficits face particular challenges unique to them. It is through communicative interactions that individuals are able to transcend the barriers erected by disability. Being unable to speak creates special problems. A well-used communication aid can be an effective tool for integrating people with communication disabilities into the culture of a particular workplace. (Dickerson L. 1995)
And language remains our greatest treasure, for without it we are confined to a world that, while not one of social isolation, is surely one that is a great deal less rich. Language makes us members of a community, providing us with the opportunity to share knowledge and experiences in a way no other species can. (Dunbar R. 1996)
Communication is the basis of learning. Communication is essential for the acquisition of knowledge. How are we to tell whether an individual (with severe physical impairment) has internalised language unless s/he can communicate? It is imperative that the neurological development of language skills are given every opportunity to proceed without impediment (Jones A.P. 1996)
A stroke can take away the power of speech. My stroke left me with very poor speech. On good days I can make myself understood but on bad days I have no speech at all. I have worked with AAC (Alternative and Augmentative Communication) throughout my working life. I have taught AAC, designed and developed AAC, marketed AAC, and lectured on AAC all over the world. After the stroke I became a consumer of AAC. I am probably the only person in the world to have occupied each of those roles. The irony of becoming a user of AAC is not lost on me. While in hospital I used a combination of very poor natural speech, my V-Pen and board, Makaton signing, and writing in a notebook at various times in order to communicate and get what I needed to say across to others. Makaton signing is tailored for use with two able hands, I only had one functioning upper limb following the stroke and even that was not very able. I had to use Makaton creatively, adapting signs made using two hands into a single handed form. It would not have mattered if I had the use of my left hand however because none of my nurses knew any Makaton. I had to teach them some signs by signing a single word and then writing down its meaning in my notebook. A very slow way to communicate! I also used my V-Pen and board. The V-Pen is a clever pen-shaped device that can recognise symbols and speak their meaning when a symbol is touched. I was involved in the system's development when I worked for Unlimiter in Taipei, Taiwan. The nurses were more interested in the Pen, it's technology, and how it worked than what I was trying to say. Many times I forgot my intended message because I became distracted in performing to an audience of nurses showing them the Pen! I had built several communication boards for use with the Pen whilst in Taiwan which I had at home. My wife brought them for me when she came to visit. While the V-Pen was a perfect AAC system for use in hospital, unfortunately the boards that I designed were not! They did not have the vocabulary necessary for use on a hospital ward.I busied myself with the design of a board that would be highly suited for this purpose and could be available on every hospital ward throughout the world. The V-Pen system is perfect for that situation because it is small, portable, and requires virtually no learning; a person could learn to use it in seconds. The spelling board option can say virtually anything provided the Patient can spell. Put that together with a couple of symbol boards and you have a really good communication system for nurses to loan to Patients during their hospital stay.
Yes, communication matters. My lack of effective communication let me down on several occasions during my time in hospital. Some are detailed on this web page. I continue to have communication difficulties nearly a year post-stroke. I guess I will have them for the remainder of my life. Silence is not golden despite what the song says. I am already beginning to notice subtle differences in the way I am treated by others. Others are uncomfortable with silence and, as I take longer to respond to communication from other people, will 'jump in' and continue communicating in what, I presume, is an effort to ease the discomfort that I must be feeling not being able to communicate effectively.There have been other barely perceivable changes too. I will not list them here but rather attempt to cover each of them in the points that I make on the remainder of this page.
I am going to have to think about my primary mode of communication for the future if my speech continues to fail me. I have considered the development of a one-handed Makaton signing system which I have tentatively called 'Maka-One'. I have not discussed my idea with the team at Makaton yet, they may not like my idea. Presently, that is all it is, an idea. There are a few single-handed sign languages already in existence (I believe Irish Sign Language is among them) but, I would have to learn them. I already know Makaton and have started adapting it for my own personal use. I believe Beyoncé has a song about it whose lyrics are something like “All the single handers, all the single signers, if you like it then you shoulda put a patenting on it”. Well, it is something near to that, I think!! Seriously, signing with just a single available hand is no joke! Having to use my one good arm and hand for everything is putting a strain on it and I am already beginning to notice it is starting to feel uncomfortable in use and it is hurting a little to bend my fingers into a fist. This is somewhat worrying for future signing, for instance. I try to take it easier but, then, I have no hands and how do I interact with my environment? I spend a great deal of the average day completely on my own, alone in bed in a room unable to get out of bed and do any of the things I used to take for granted. I have an emergency contact button which, if I were to use it, would contact an outside service to summon help. In such a situation, my speech would certainly fail me. It is good that the line knows who and where I am and has the details of emergency contacts, even if I could not say a word during any use. The service is not free, it costs me around £20 per month. Disability doesn't come cheap in 2021. I suspect it has always been so.

9. Sign of the times. All Carers should know some basic (Makaton) signs, such that they will be able to understand if a Client is trying to communicate, or to be able to demonstrate to a Client how to make basic communication; for example, how to sign ‘yes’ and ‘no’. If sign is not known to the Carers, ask the Client to demonstrate some basic signs. I was signing ‘I don’t know’ this morning slowly several times. The Carers, rather than see my signs as an answer to the question they had just asked of me, decided that I was pointing out that my chest needed washing. They hadn’t a clue and seemingly preferred to remain ignorant of ways to make any communication between us a lot better. Communication matters - Always attempt to establish a meaningful means of communication for and with the Client. It may be that the Client utilises an alternative form of communication (for example, a sign or symbol system). In which case, attempt to learn how able s/he is in its use. If you are not competent in sign language, ask your Client to show you how s/he makes basic signs. For example, yes, no, please, thank you, pain and any others that it might be useful to know. Be a little wary of copying a Client’s signs without checking that the sign is correct. While it is acceptable for a Client to use idiosyncratic signing (for example, I only have use of my right hand and so I have adapted my knowledge of Makaton to work with only one hand) (Note: I believe Irish Sign Language only requires the use of one hand), idiosyncratic signing is not acceptable for the Carers! Playing Chinese Whispers with sign language is sure to result in very strange hand movements recognisable by no one. Learn to recognise the signs as used by the Client. It can be very frustrating for a Client, when signing, if the Carers do not comprehend the message. A good place to learn some basic (Makaton) signs is to search for ‘Mr Tumble’ videos on YouTube. ‘Mr Tumble’ is not just for children. Everyone should know some signs: schools should teach sign language. Sign language should be an option on the curriculum alongside French and German. If the Client has apparently no recognisable means of communication, and a significant cognitive impairment, it is possible to attempt to turn an already existing behaviour into a meaningful mode of communication (Ware 2012). For example, if the Client is able to move any part of his / her anatomy purposefully, it may be possible to associate that particular movement with a specific concept by always responding to it in exactly the same way. Moving a hand slightly to the right (or slightly lifting a finger) might be taken to mean ‘yes’, for example. The consistency of the response establishing a relationship, over time, such that a movement, which a Client was already capable of performing, becomes an idiosyncratic sign for the word. It is very important that all involved with the Client respond consistently, in the same way, to establish the link. Significant Others should be aware of all that is attempted. Where a Client has an existing method of alternative communication, it is very important that Carers do not impede its access for any longer than is essential. A symbol book or chart may need to be out of the way, while rolling, for example, but the Client should have access to it as soon as possible after. Do not deprive the Client of a means of communication for longer than is necessary.
Update (15th Aug '21): This morning the Carers asked me a question. By the time I had the chance to answer in sign, they had already asked several more questions. I signed "I don't know". The Carers hadn't got a clue what I was saying. They would not know which of the questions they had asked to which my signing was the response, because they had moved on so far beyond the original question. In the end, my wife had to come and act as an interpreter to prevent them from carrying out an unnecessary task based on an incorrect assumption of the meaning of my signing.
Update (15th Aug '21): This morning the Carers asked me a question. By the time I had the chance to answer in sign, they had already asked several more questions. I signed "I don't know". The Carers hadn't got a clue what I was saying. They would not know which of the questions they had asked to which my signing was the response, because they had moved on so far beyond the original question. In the end, my wife had to come and act as an interpreter to prevent them from carrying out an unnecessary task based on an incorrect assumption of the meaning of my signing.

10. Don't ask her, ask me. As previously noted, questions on care should be addressed to the Client and not to some other member of the Client’s family. It is truly demeaning to Clients to ignore them completely and address questions to others. It is the old ‘does he take sugar?’ issue (Wagner 1991; Hogg & Wilson 2004). Radio 4 (UK) used to broadcast a weekly series entitled ‘Does He Take Sugar?’ (It started in 1977 and ran for about twenty years) in which it covered the treatment of the disabled. The title of the program refers to an all-to-frequent occurrence, in which a person asks another (other than the person with the disability) a question about a topic avoiding talking to the person with the disability. People often discuss items concerning someone with a disability, while s/he is present, and do not include the person even though s/he can speak for him / herself. The radio series made this type of thing explicit and gave People Of Disability (POD) a voice. My wife has replied to people, behaving in this fashion, on several occasions,
“I don’t know. Why don’t you ask him?”
Always address questions to Clients. Even if incapable of verbal communication, the Client may still be able to respond using an alternative methodology. If another family member is around, they are likely to respond on the Client’s behalf if they know the Client is unable to answer for himself / herself for any reason. The Client will always appreciate that the Carers directed question at him / her even though s/he is not able to reply in a comprehensible fashion in the situation. Bypassing the individual completely is both demeaning and very poor practice. If a Client responds in a manner that is incomprehensible, never denigrate the Client’s response system,
“Oh, I don’t understand those stupid signs, can you write it down?”
Rather say,
“I am sorry John, I never learned any sign language, but perhaps you could teach me how you say some basic things when I come the next few times and you will help me to understand you better. Is that OK with you? Does the sign you are making mean Yes?”
“I don’t know. Why don’t you ask him?”
Always address questions to Clients. Even if incapable of verbal communication, the Client may still be able to respond using an alternative methodology. If another family member is around, they are likely to respond on the Client’s behalf if they know the Client is unable to answer for himself / herself for any reason. The Client will always appreciate that the Carers directed question at him / her even though s/he is not able to reply in a comprehensible fashion in the situation. Bypassing the individual completely is both demeaning and very poor practice. If a Client responds in a manner that is incomprehensible, never denigrate the Client’s response system,
“Oh, I don’t understand those stupid signs, can you write it down?”
Rather say,
“I am sorry John, I never learned any sign language, but perhaps you could teach me how you say some basic things when I come the next few times and you will help me to understand you better. Is that OK with you? Does the sign you are making mean Yes?”

11. Inclusive talking. I have found that Carers in pairs tend to talk to each other most of the time and not to me! Talk should always be inclusive; that is, involving the Client. Even if the Client is a poor communicator, that is not an excuse for excluding him / her. If the Client cannot speak at all, try to involve the person in conversation and expect signed, symbolic, facial, vocal sound, or body language responses. Try to talk about topics in which the person is interested: their previous job or pastime, favourite TV programme or films or music, the local or national news, a sporting event, family matters, etc. Do not talk over them, talk to them. Never talk about a Client unless you are talking to the Client. Never discuss matters about another Client in the presence of a Client. That is unprofessional. It is acceptable practice to ‘tell by indication’ (pointing to or touching very gently) especially if the Client has learning difficulties or is in any way intellectually impaired and has problems in understanding spoken language. Thus, when informing a Client of the need to move his arm, it is acceptable to enhance the likely understanding of spoken language by pointing to or, if required, gently touching the arm briefly. If a Client does not communicate, it may be necessary to contact the local speech therapy service for support. The Client’s Care Plan should detail the Client’s Speech and Language Therapist if one is already supporting the Client. The SLT may be able to advise on a suitable AAC (Alternative or Augmentative Communication) system should it prove necessary.
12. Talk to me. If a Significant Other is present while performing care duties, ensure that any conversation is with the Client and not with the Other without including the Client. It is not good practice to talk about the Client with another while the Client is present and can overhear especially if the talk refers to something negative. Do not discuss, with the second Carer, the details of the coming day. Do not talk about other Clients (their information is private). Even if your Client is not very talkative, you should still talk to them and include them in the conversation. The main topic of conversation amongst the nursing staff in hospital (conversations that did not include me) appeared to be concerned with details of shift rota or the details of their next break. Nurses would typically carry on a conversation concerning shifts while working with a Patient, talking between themselves across a Patient. The Patient may as well not have been there!
13. A dumb person. As a result of the stroke, my speech was impaired. Sometimes, I can hardly speak at all: when I am emotional, when my mouth and throat are dry (usually following sleep), when my throat needs clearing (since the stroke, I cannot cough on demand (I have to wait until it happens naturally)) and, at other times, for reasons I cannot explain. At each of these times, I resort to single-handed sign language until I am able to speak once again. Just because I am ‘struck dumb’ occasionally, it does not follow that I become periodically intellectually incapacitated. Never talk to a Client as though s/he is cognitively deficient, presume intelligence until confirmed otherwise. Even then, always be respectful and communicate with the Client in a manner suited to, and commensurate with, her / his abilities.
Think on these words
As these pages you thumb, for
Speechless is not Thoughtless
And Voiceless not Dumb
(Jones 1996)
As these pages you thumb, for
Speechless is not Thoughtless
And Voiceless not Dumb
(Jones 1996)
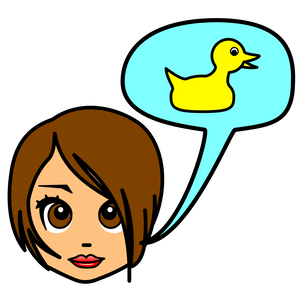
14. Terms of endearment. Always call the Client by his / her given first name or by their preferred name. Never use terms such as sweetheart, sweetie, darling, flower, petal, duck, m' duck, ducky, my love, hun, etc. I have been addressed by each of these terms during the past eleven months. While I am not offended by the use of such terminology, I would much prefer that Carers used my name; it is no more effort. Carers are not in a romantic relationship with the Client so they should use the Client’s preferred name at all times (Comerford 2015; Laskowski-Jones 2015). It is also necessary for Carers to use age appropriate language at all times. “Good boy” is not appropriate for an adult male.
When I am eating my wife puts a tea towel across my chest such that if I accidentally drop any hot food it falls onto the towel and not my bare flesh. Once, the Carers arrived before I started my lunch but after the towel was in place:
1st Carer: "Oh! You've got your bib on ready for dinner."
Me (struggling to speak) "Don't call it a bib. I am an adult."
2nd Carer to 1st Carer: "What did he say?"
1st Carer to 2nd Carer: " I haven’t a clue" (and starts the normal lunch visit procedure with no attempt to ask and clarify my statement.)
The use of inappropriate language is covered further in the eating and drinking section later on this page.
What’s in a name? That which we call a rose
By any other name would smell as sweet
(Shakespeare. Romeo and Juliet, II, ii)
(Levenson, J. 2000).
A linguistic sign is not a link between a thing and a name, but between a concept and a sound pattern. The sound pattern is not actually a sound; for a sound is something physical. A sound pattern is the hearer’s psychological impression of a sound, as given to him by evidence of his senses. This sound pattern may be called a ‘material’ element only in that it is the representation of our sensory impressions. The sound pattern may thus be distinguished from the other element associated with it in a linguistic sign. This other element is generally of a more abstract kind: the concept
(De Saussure F. 1916 pp 98)
Words Wittgenstein now insisted, cannot be understood outside the context of the non-linguistic human activities into which the use of the language is interwoven .... the way to understand the meaning of a word is to study it in the language-game to which it belongs, to see how it contributes to the communal activity of a group of language-users. In general, the meaning of a word is not an object for which it stands, but rather its use in a language.
(Kenny A. 1973 page 14)
It’s only for a small minority of words that we can give definitions without these fuzzy edges. Until recently, the metre was officially defined as the distance between two particular scratches on a particular metal bar kept in a particular vault in Paris, and, if you wanted to know if your metre stick was a metre long or not, all you had to do was to take it to Paris and lay it alongside that bar. This works pretty well for metre, but it wouldn’t work for most other words: we could hardly keep a standard dog in a vault to compare against candidate dogs, or a standard chair, or a standard smile.
(Trask R. 1995 Page 50)
By any other name would smell as sweet
(Shakespeare. Romeo and Juliet, II, ii)
(Levenson, J. 2000).
A linguistic sign is not a link between a thing and a name, but between a concept and a sound pattern. The sound pattern is not actually a sound; for a sound is something physical. A sound pattern is the hearer’s psychological impression of a sound, as given to him by evidence of his senses. This sound pattern may be called a ‘material’ element only in that it is the representation of our sensory impressions. The sound pattern may thus be distinguished from the other element associated with it in a linguistic sign. This other element is generally of a more abstract kind: the concept
(De Saussure F. 1916 pp 98)
Words Wittgenstein now insisted, cannot be understood outside the context of the non-linguistic human activities into which the use of the language is interwoven .... the way to understand the meaning of a word is to study it in the language-game to which it belongs, to see how it contributes to the communal activity of a group of language-users. In general, the meaning of a word is not an object for which it stands, but rather its use in a language.
(Kenny A. 1973 page 14)
It’s only for a small minority of words that we can give definitions without these fuzzy edges. Until recently, the metre was officially defined as the distance between two particular scratches on a particular metal bar kept in a particular vault in Paris, and, if you wanted to know if your metre stick was a metre long or not, all you had to do was to take it to Paris and lay it alongside that bar. This works pretty well for metre, but it wouldn’t work for most other words: we could hardly keep a standard dog in a vault to compare against candidate dogs, or a standard chair, or a standard smile.
(Trask R. 1995 Page 50)
This is also true of the signs used by the deaf community: there may be some signs that are iconic and are either transparent or translucent but the majority are simply opaque:
although sometimes signs partly depict what they refer to, hardly ever are the forms of signs completely determined by what they mean. So ASL vocabulary has to be learned just like that of a spoken language
(Jackendoff R. 1993 page 89)
(For ASL read BSL or any other sign language)
(Jackendoff R. 1993 page 89)
(For ASL read BSL or any other sign language)
Both signs and words only have a dictionary definition outside of the particular context in which they were uttered. Rarely do the words used in spoken language exactly conform to a dictionary definition. They can only be truly understood with an insider’s knowledge of the political and social narrative of the speaker and a knowledge of the context in which they were spoken. There is presently a lot of fuss in the media concerning the use of appropriate pronominal forms. I am not 'woke' but I would prefer the use of 'he' when it comes to talking about me in the third person. I identify as male because I am a man. As a white male, I do not consider that I have 'privilege'. I would swap my present existence with almost any other person if it is their belief that I have such 'privilege'. My best guess is that there will not be many people in the queue to be me right now. It is my opinion that the queue would be very short indeed. I have no problem with being identified as a POD, because that is what I am, a Person Of Disability. I do not require a special term of reference, 'he' is just fine.
"Tony? Oh he's the POD who has had a stroke."
I am what I am - first a 'person' and second I have a disability. I would not be offended by any person's recognition that I am disabled, although I would not want that to be the first description of me. I am a person first and my disability is definitely in second place. I am not a DOP, a Disability Of Personality. I would not like to be thought of as a disability first. My disability does not define me, I define my disability except for the times when I am in serious pain. Then, my disability really does define who I am.
"Tony? Oh he's the POD who has had a stroke."
I am what I am - first a 'person' and second I have a disability. I would not be offended by any person's recognition that I am disabled, although I would not want that to be the first description of me. I am a person first and my disability is definitely in second place. I am not a DOP, a Disability Of Personality. I would not like to be thought of as a disability first. My disability does not define me, I define my disability except for the times when I am in serious pain. Then, my disability really does define who I am.
I am a POD not a DOP. I would prefer to be treated in that way.

15. Questions, questions. (Ward, Kibble et al 2013; Myers 2019; Institute for Healthcare Improvement 2021) When talking to a Client only ask one question at a time. When more than one person is asking questions, it can become terribly confusing for the Client who does not know which question, from which person, to answer. Only one person should be asking simple questions, one at a time, and the person should wait for a response before asking another. A frightened, bewildered, or in-pain Client requires calm, not a barrage of questions from over-anxious Carers.
“Where’s it hurting?” - “Is it your leg?” - “Do you want me to get the doctor?” - “Do you want us to move you?” - “Are you feeling sick?” - “Do you feel hot?” - “What can I do to help?”
“STOP asking so many questions all at once!”
“Where’s it hurting?” - “Is it your leg?” - “Do you want me to get the doctor?” - “Do you want us to move you?” - “Are you feeling sick?” - “Do you feel hot?” - “What can I do to help?”
“STOP asking so many questions all at once!”
16. Deaf and dumb? (Birbeck Nevins 1895) Some Clients may be hard of hearing. It does not follow that this is a licence to shout. Rather, the Carer should get in a position such that the Client is able to see her / his face clearly. The Carer should not stand with her / his back to a window such that the light coming in puts the Carer’s face in the shade (De Weerdt & Kusters 2016). The Client may be able to gather information to comprehend the situation from body language and the movement of a Carer’s lips and mouth. If Carers know a little sign language, please make use of it. Even if the Client does not know how to sign, your use may assist understanding as well as teaching the sign.
Client Care and Care Practice

17. Phone protocol. Never make or take a phone call while with a Client unless calling for medical aid (or in an emergency) and then only with the Client’s permission. Taking a personal call is unprofessional; wait until not with a Client and then call back, if the call was important. Turn off phones while with a Client. I have witnessed Carers taking calls from family members, friends, and even the Care Company during the time I am paying for care! Care Companies should not ring staff during the time that they are attending a client. It is completely unprofessional. They should develop a system such that they are able to contact staff between Client calls.
18. Idle hands. It is bad practice to sit or stand around Idle not doing anything or chatting with a colleague. This is especially true if the Client is paying for the service. While waiting for the Client to complete a task, Carers should be productive. Are there cleaning or tidying tasks? The Client can tell the Carers when s/he has finished the task. In that way, Clients are in control. This morning, two Carers stood idly chatting to one another while I washed my face with a flannel using my good arm. I take my time when washing my face because I don’t shave. The left side of my mouth feels like it used to after a visit to the dentist and given an injection to numb the pain. It feels like that except it never wears off. When I eat, food tends to escape from the left half, unbeknownst to me and gets trapped in my beard and dries hard in place. As such, it takes a while for me to clean when washing. I noted the time that the Carers did nothing but chat as I washed my face. After five minutes had elapsed and they still were Idle, I stopped what I was doing and asked,
“Why are you just standing there?”
They ‘explained’ that they were waiting for me to complete washing my face! I have to pay for this service. It is not free. While five minutes does not sound much, the call is only for thirty minutes total. The Carers could wash my legs and my abdomen whilst I wash my face. Attached to my legs are my feet yet, my feet were not washed at all and, two quick wipes of my legs hardly qualifies as ‘washing’. Five minutes idle and other things performed poorly. This is not good practice. Later, in that same session, I informed the Carers that this is the day that I have my hair washed. The Carers did not like this and asked my wife if ‘tomorrow’s Carers’ could do it instead. Asking my wife, and not me, is simply poor practice, let alone not wanting to do what their Client had asked! What I was asking did not break the ‘dubious’ rule (see point 4) and, therefore, the Carers ought to have performed the task.
“Why are you just standing there?”
They ‘explained’ that they were waiting for me to complete washing my face! I have to pay for this service. It is not free. While five minutes does not sound much, the call is only for thirty minutes total. The Carers could wash my legs and my abdomen whilst I wash my face. Attached to my legs are my feet yet, my feet were not washed at all and, two quick wipes of my legs hardly qualifies as ‘washing’. Five minutes idle and other things performed poorly. This is not good practice. Later, in that same session, I informed the Carers that this is the day that I have my hair washed. The Carers did not like this and asked my wife if ‘tomorrow’s Carers’ could do it instead. Asking my wife, and not me, is simply poor practice, let alone not wanting to do what their Client had asked! What I was asking did not break the ‘dubious’ rule (see point 4) and, therefore, the Carers ought to have performed the task.

19. A good listener. Give the Client the opportunity to provide feedback on your practice. Towards the end of the session you might ask the question,
”John We would like to know how we have done this time. Would you tell us anything that we can do better or concerned you with what happened during our visit?”
Do not be defensive during any feedback, rather listen attentively and not interrupt. Thank the Client for the feedback and say that you will take on board the comments for future practice. Remain calm even if you believe the Client’s comments to be false. Anger and or sarcastic comments will not help the situation. Attempt to act on the feedback during subsequent sessions.
”John We would like to know how we have done this time. Would you tell us anything that we can do better or concerned you with what happened during our visit?”
Do not be defensive during any feedback, rather listen attentively and not interrupt. Thank the Client for the feedback and say that you will take on board the comments for future practice. Remain calm even if you believe the Client’s comments to be false. Anger and or sarcastic comments will not help the situation. Attempt to act on the feedback during subsequent sessions.
20. Incontinence is not just inconvenience. Being doubly incontinent is a pain, both figuratively and literally. It is more than an inconvenience; it is annoying, bothersome, costly, demeaning, embarrassing, painful, potentially harmful, odorous, time-consuming, troublesome, and worrying. I used to be able to ‘skip to m’ loo’ whenever the urge arose, now I have such poor control over these functions that I require a catheter for one and a daily suppository for the other (number two, pun intended). Since having my catheter, it has caused me nothing but pain and problems. The stroke has messed up my bowels. An event that normally is a very private affair became very public overnight. It requires a-n-other to clean up the mess (literally) and that is both demeaning and embarrassing. Carers are usually very good in this role. It cannot be very pleasant and, as I can attest, the Client does not relish the process either; it is something I would much rather do all by myself if I could. It is very good practice to perform such duties as quickly and with as little fuss as possible for both the Carers and the Client. The Client is not happy that others have to perform this duty and will be very grateful if Carers can make it as routine as possible. Prepare all that is likely to be needed in advance such that time is not taken searching for a necessary item and slowing the process. Remember, continual wiping with a wet-wipe may result in making an area sore. Be as gentle as possible.
Evacuating the bowels requires the ability to bear down, to 'push' faecal matter out. After the stroke I could no longer do this. This inability caused me great pain and a lot of anxiety. It wasn't helped by the staff in the stroke unit not appearing to understand my condition and constantly telling me to do something that I physically was no longer able to do. My problem continued after I was discharged from hospital and was back at home. I spent hours screaming in pain and begging my wife to get me some help on more than one occasion. The pain was so intense that I repeatedly asked to die, I saw no future beyond more pain. Although we called the local surgery many times, the doctors there displayed no urgency in helping. On the one occasion that a doctor from the surgery came out to see me in ten months following my stroke, he simply gave me an enema and left quickly. It was as though he couldn't get out of the house fast enough. His action was nothing that my wife could not have done herself. There was no in depth discussion of my condition. I was left to fight the problem together with my wife and face the prospect of even more pain. Over the months we started to resolve the issue with daily use of strong suppositories and frequent intake of laxatives. That remains the situation to this day. It is not ideal but at least I am no longer screaming in pain.
Being in continual pain occupies the mind to the exclusion of virtually everything else. I did not want to talk to anyone, I did not want to write emails, I did not want to watch television. The pain consumed my whole being. I wanted for it to end even if it meant ending my life. Today, I am on a pain management scheme mostly initiated by myself. I saw a morphine pain patch in use on another Patient while in hospital and I told my doctor at home that is what I wanted. I found out about neuropathic medication from a conversation with my physiotherapist and asked her to contact my doctor to get him to prescribe daily amitriptyline. I should have been prescribed it from the start but the pain medication that I was on was not doing anything for me. Every piece of medication that I now have for pain was not suggested by my doctor, it came because I asked for it. Well, if truth be told, my wife did on my behalf. I have an existing AAC system, it is called a wife!
I have a continuing battle with my catheter. It is the cause of even more pain. The nurses suggestion for pain relief? Take paracetamol. Paracetamol is virtually ineffective for catheter and urinary pain. The nurses other advice? Drink more water. I have problems swallowing and drinking has been a real issue for me. I drink as much as I am able. To be told to drink more shows a lack of understanding of my condition. In the hospital when the catheter seemed to be causing me pain, I asked for it to be cleaned in case it was blocked. Eventually, a nurse flushed the catheter and it appeared to work in that the pain ceased. Thus, when I was at home and my catheter started causing me similar pain, I asked for it to be flushed. I finally got my first catheter flush this week after ten months of asking and many catheter changes and more hours screaming in pain. I could be screaming in pain for in excess of three hours before an emergency nurse came to answer my wife's pleading call. Even then, the nurses were reluctant to change my catheter telling me to
"take Paracetamol and drink more"
but, in the end, they always changed the existing catheter for a new one. Once it had to be done twice in the same visit. I don't know if you have ever had a catheter fitted but it is not the most pleasant of experiences and, yet, I welcomed the process as it usually meant instant relief from the pain. I am told by my Carers that other of their Clients also have continuing catheter issues. There ought to be some sort of solution to the issues caused by catheters, such that, when fitted, they can act to prevent problems instead of reacting to them at the cost of pain and misery for the Client.
Pain in one area of my body usually sets off a chain reaction leading to pain in a separate area entirely. When I am in pain it causes the muscles in my left arm to contract. My fingers curl tightly into a fist and my arm moves across and up my chest eventually punching me under my jaw. Moving it back by my side becomes ever more painful as the muscles stiffen. Pain causes my leg to spasm and the muscles in my left foot to tighten and twist my foot into a shape that it clearly doesn't like because it reacts with even more pain. My leg might continue spasming for several minutes, during which time I try to focus on some specific task on my computer in an attempt to ignore (at least, help me to get through) the pain. I am daily doses of Baclofen to suppress the spasms and relax stiffening muscles as well as quarterly injections of the maximum amount of Botox permissible. Many people would pay a lot of money for the Botox injections I receive every three months. The injections use a very long needle pushed into my arm and leg in several spots. It is not a pleasant procedure. I would not pay to have it done as some do for vanity. My physiotherapist, who is brilliant, says that she can feel a difference in my muscles but it still hurts like crazy when she bends my arm and leg to and thro. Although I need to see her at the very least once a week, she has to cut down her visits to once in three weeks and I have no doubt that I will see her less and less. I really need regular weekly physiotherapy to keep my limbs from further degeneration but that is not what I am getting. Post-stroke provision is not good in my area. I could pay for private physiotherapy but I am already paying tens of thousands of pounds for other necessary services and I simply cannot afford to go on spending at my current rate. Furthermore, I have paid a life time into health provision in the form of National Insurance contributions and have taken very little out until my recent spell with the NHS following the stroke. I would think that I have already paid for physiotherapy treatment.
Last evening, a little after six o'clock I started to have catheter pains. It is intense pain that comes in waves approximately every fifteen minutes (often less) and lasts for a excruciating minute before subsiding over about another minute or so. My wife changed my leg bag to monitor the flow of urine and, because I was still in so much pain, rang the nursing service at a little before midnight to ask for a nurse to come and take a look at my catheter. The nursing services said a nurse would call back and arrange a visit. Almost an hour later, a nurse called and, after discussing my problem over the phone, said that I needed a doctor. The nurse said that she would contact the out-of-hours doctor and he would call to arrange a visit. This might take up to two hours. Three hours later, a man called and discussed my problem over the phone. He eventually said that he wasn't a doctor, he was a clinician. However, he said that he could not help, I needed a doctor. He said that he would contact a doctor and get him to call. It probably would take about an hour. Over an hour later, a doctor called and, once again, we (my wife as my voice is not good enough for a phone conversation) discussed my issues over the phone. The doctor concluded that the problem was with my catheter and it needed to be flushed. A nurse would have to do it. He would arrange for a nurse to call. Another hour passed. A nurse called and discussed the problem and said that she did not flush catheters and would arrange for another nurse to call. Another hour passed, a nurse called. she said, as my urine was going into the leg bag, there wasn't a blockage and I needed to contact my own doctor. She said that there was a daytime visit scheduled and they would flush my catheter and take a sample to test for an infection. I was livid! Both myself and my wife had been awake all night and I was still suffering with intense pain every fifteen minutes or so. We had been passed from pillar to post with everyone saying something different and, twelve hours later, we were no further on than when we started. I was in pain but no-one took responsibility for helping me. The system was a complete failure. I would have to wait till the nurses came during the day and the problem might be resolved. I have no choice but to wait even longer. I just hope that the pain is not as intense during this time.
Update: I remained in pain all through that morning, still nobody came. At the lunchtime Carers call, they noticed that the catheter had come out completely. It is not supposed to do that. Obviously the balloon part of the catheter inside my bladder had burst and there was nothing holding the catheter in place. It had been gradually coming out throughout the night and that was causing my problems. The Carers called nursing services and they said they would send someone. It was three phone calls later at almost two o'clock in the afternoon that a nurse finally came and fitted a new catheter. The pain went away. It had been nearly fourteen hours and many phone calls to get me some help. Why couldn't someone have come when we first called and saved me hours of agony? Having a stroke is just the beginning of the nightmare. Note: the Carers were brilliant and did everything correctly. They called nursing services on seeing my distress. Praise where praise is due.
Update #2. The new catheter came out again! It was only two days after the first new catheter was fitted. The same level of pain during the time it took to happen a second time. A nurse came and fitted another catheter. She recommended that, if it happened again, I should request a catheter with a bigger balloon.
Update #3. Two days after the second catheter was fitted I started to have the same pains. Again, a nurse was called. When she arrived my wife explained in detail all that had passed before. The nurse took one look at my catheter and said that, as it was still in and was draining, there was nothing that she could do. Pain was an issue for my doctor. After that, the nurse applied some gel which was supposed to help numb the pain and left. The gel did nothing to ease the pain. Ten minutes after the nurse left, another wave of pain commenced.
Update #4. A day later my wife called the doctor's surgery to book a telephone appointment. Later that day the doctor called and, after explaining my issue and all that had happened, the doctor decided that I needed a home visit to try and establish the cause of the pain. Someone would come and see me the following day. The next day a nurse practitioner came (not a doctor). She said straight away that she wasn't equipped to do a urine test and would arrange for another nurse to come and do that. She also said that she would prescribe some cream and some stronger pain medication. To date (two days later) no nurse has been to perform the test. The nurse has not prescribed the stronger pain medication as she said, My wife is going to the surgery to try and establish what has happened. Meanwhile, I still am having the same pain, and bypassing the catheter quite a lot. I have been in pain for five days now. This situation has been going on for months with no long term resolution. New catheters, when fitted, stop the pain for a few days, perhaps a week, but the same pain always returns. Whatever is causing the pain has not been resolved. All that happens is I am given something to mask the pain. What I need is an identification of the cause and a cure. The pain is worse today.
Update #5 (5th Aug. '21). It has been six days since my wife first reported my situation. My pain has moved from coming in waves to continual. Today a nurse came to test my urine for an infection. The test was positive. Why has it taken six days for this to happen? Six days of pain. My condition getting worse.It is taking a lot of effort and quite some time to type this. The nurse is going straight to the doctor's surgery to get antibiotics prescribed and to refer me to urology at the hospital urgently. Perhaps now, something will be done to help sort this ongoing issue after eleven months and the current occurrence of almost a week in pain.
Update #6 (6th Aug'21). I have started a course of antibiotics and have a larger morphine patch. The pain has finally gone. I suspect it will return in a week or so but I hope it won't. It has returned in the past to torment me time and time again. When I think it has gone and the future looks brighter, the pain returns after a short break when I am pain free. Then, I have a further problem with my catheter or I contract another UTI or something else happens and the pain is back again. Doctors and nurses typically treat the symptoms and not the cause. I don't think they know what is causing my repeated bouts of pain. A nurse is scheduled today to change my catheter to help with the fight against my latest UTI. I will provide a further update at some future date to explain how things work out.
Update #7 (14th Aug '21) I have been pain free for several days now and my catheter seems to be behaving itself. A few days without pain is a good thing for me. I hope that this continues.
Evacuating the bowels requires the ability to bear down, to 'push' faecal matter out. After the stroke I could no longer do this. This inability caused me great pain and a lot of anxiety. It wasn't helped by the staff in the stroke unit not appearing to understand my condition and constantly telling me to do something that I physically was no longer able to do. My problem continued after I was discharged from hospital and was back at home. I spent hours screaming in pain and begging my wife to get me some help on more than one occasion. The pain was so intense that I repeatedly asked to die, I saw no future beyond more pain. Although we called the local surgery many times, the doctors there displayed no urgency in helping. On the one occasion that a doctor from the surgery came out to see me in ten months following my stroke, he simply gave me an enema and left quickly. It was as though he couldn't get out of the house fast enough. His action was nothing that my wife could not have done herself. There was no in depth discussion of my condition. I was left to fight the problem together with my wife and face the prospect of even more pain. Over the months we started to resolve the issue with daily use of strong suppositories and frequent intake of laxatives. That remains the situation to this day. It is not ideal but at least I am no longer screaming in pain.
Being in continual pain occupies the mind to the exclusion of virtually everything else. I did not want to talk to anyone, I did not want to write emails, I did not want to watch television. The pain consumed my whole being. I wanted for it to end even if it meant ending my life. Today, I am on a pain management scheme mostly initiated by myself. I saw a morphine pain patch in use on another Patient while in hospital and I told my doctor at home that is what I wanted. I found out about neuropathic medication from a conversation with my physiotherapist and asked her to contact my doctor to get him to prescribe daily amitriptyline. I should have been prescribed it from the start but the pain medication that I was on was not doing anything for me. Every piece of medication that I now have for pain was not suggested by my doctor, it came because I asked for it. Well, if truth be told, my wife did on my behalf. I have an existing AAC system, it is called a wife!
I have a continuing battle with my catheter. It is the cause of even more pain. The nurses suggestion for pain relief? Take paracetamol. Paracetamol is virtually ineffective for catheter and urinary pain. The nurses other advice? Drink more water. I have problems swallowing and drinking has been a real issue for me. I drink as much as I am able. To be told to drink more shows a lack of understanding of my condition. In the hospital when the catheter seemed to be causing me pain, I asked for it to be cleaned in case it was blocked. Eventually, a nurse flushed the catheter and it appeared to work in that the pain ceased. Thus, when I was at home and my catheter started causing me similar pain, I asked for it to be flushed. I finally got my first catheter flush this week after ten months of asking and many catheter changes and more hours screaming in pain. I could be screaming in pain for in excess of three hours before an emergency nurse came to answer my wife's pleading call. Even then, the nurses were reluctant to change my catheter telling me to
"take Paracetamol and drink more"
but, in the end, they always changed the existing catheter for a new one. Once it had to be done twice in the same visit. I don't know if you have ever had a catheter fitted but it is not the most pleasant of experiences and, yet, I welcomed the process as it usually meant instant relief from the pain. I am told by my Carers that other of their Clients also have continuing catheter issues. There ought to be some sort of solution to the issues caused by catheters, such that, when fitted, they can act to prevent problems instead of reacting to them at the cost of pain and misery for the Client.
Pain in one area of my body usually sets off a chain reaction leading to pain in a separate area entirely. When I am in pain it causes the muscles in my left arm to contract. My fingers curl tightly into a fist and my arm moves across and up my chest eventually punching me under my jaw. Moving it back by my side becomes ever more painful as the muscles stiffen. Pain causes my leg to spasm and the muscles in my left foot to tighten and twist my foot into a shape that it clearly doesn't like because it reacts with even more pain. My leg might continue spasming for several minutes, during which time I try to focus on some specific task on my computer in an attempt to ignore (at least, help me to get through) the pain. I am daily doses of Baclofen to suppress the spasms and relax stiffening muscles as well as quarterly injections of the maximum amount of Botox permissible. Many people would pay a lot of money for the Botox injections I receive every three months. The injections use a very long needle pushed into my arm and leg in several spots. It is not a pleasant procedure. I would not pay to have it done as some do for vanity. My physiotherapist, who is brilliant, says that she can feel a difference in my muscles but it still hurts like crazy when she bends my arm and leg to and thro. Although I need to see her at the very least once a week, she has to cut down her visits to once in three weeks and I have no doubt that I will see her less and less. I really need regular weekly physiotherapy to keep my limbs from further degeneration but that is not what I am getting. Post-stroke provision is not good in my area. I could pay for private physiotherapy but I am already paying tens of thousands of pounds for other necessary services and I simply cannot afford to go on spending at my current rate. Furthermore, I have paid a life time into health provision in the form of National Insurance contributions and have taken very little out until my recent spell with the NHS following the stroke. I would think that I have already paid for physiotherapy treatment.
Last evening, a little after six o'clock I started to have catheter pains. It is intense pain that comes in waves approximately every fifteen minutes (often less) and lasts for a excruciating minute before subsiding over about another minute or so. My wife changed my leg bag to monitor the flow of urine and, because I was still in so much pain, rang the nursing service at a little before midnight to ask for a nurse to come and take a look at my catheter. The nursing services said a nurse would call back and arrange a visit. Almost an hour later, a nurse called and, after discussing my problem over the phone, said that I needed a doctor. The nurse said that she would contact the out-of-hours doctor and he would call to arrange a visit. This might take up to two hours. Three hours later, a man called and discussed my problem over the phone. He eventually said that he wasn't a doctor, he was a clinician. However, he said that he could not help, I needed a doctor. He said that he would contact a doctor and get him to call. It probably would take about an hour. Over an hour later, a doctor called and, once again, we (my wife as my voice is not good enough for a phone conversation) discussed my issues over the phone. The doctor concluded that the problem was with my catheter and it needed to be flushed. A nurse would have to do it. He would arrange for a nurse to call. Another hour passed. A nurse called and discussed the problem and said that she did not flush catheters and would arrange for another nurse to call. Another hour passed, a nurse called. she said, as my urine was going into the leg bag, there wasn't a blockage and I needed to contact my own doctor. She said that there was a daytime visit scheduled and they would flush my catheter and take a sample to test for an infection. I was livid! Both myself and my wife had been awake all night and I was still suffering with intense pain every fifteen minutes or so. We had been passed from pillar to post with everyone saying something different and, twelve hours later, we were no further on than when we started. I was in pain but no-one took responsibility for helping me. The system was a complete failure. I would have to wait till the nurses came during the day and the problem might be resolved. I have no choice but to wait even longer. I just hope that the pain is not as intense during this time.
Update: I remained in pain all through that morning, still nobody came. At the lunchtime Carers call, they noticed that the catheter had come out completely. It is not supposed to do that. Obviously the balloon part of the catheter inside my bladder had burst and there was nothing holding the catheter in place. It had been gradually coming out throughout the night and that was causing my problems. The Carers called nursing services and they said they would send someone. It was three phone calls later at almost two o'clock in the afternoon that a nurse finally came and fitted a new catheter. The pain went away. It had been nearly fourteen hours and many phone calls to get me some help. Why couldn't someone have come when we first called and saved me hours of agony? Having a stroke is just the beginning of the nightmare. Note: the Carers were brilliant and did everything correctly. They called nursing services on seeing my distress. Praise where praise is due.
Update #2. The new catheter came out again! It was only two days after the first new catheter was fitted. The same level of pain during the time it took to happen a second time. A nurse came and fitted another catheter. She recommended that, if it happened again, I should request a catheter with a bigger balloon.
Update #3. Two days after the second catheter was fitted I started to have the same pains. Again, a nurse was called. When she arrived my wife explained in detail all that had passed before. The nurse took one look at my catheter and said that, as it was still in and was draining, there was nothing that she could do. Pain was an issue for my doctor. After that, the nurse applied some gel which was supposed to help numb the pain and left. The gel did nothing to ease the pain. Ten minutes after the nurse left, another wave of pain commenced.
Update #4. A day later my wife called the doctor's surgery to book a telephone appointment. Later that day the doctor called and, after explaining my issue and all that had happened, the doctor decided that I needed a home visit to try and establish the cause of the pain. Someone would come and see me the following day. The next day a nurse practitioner came (not a doctor). She said straight away that she wasn't equipped to do a urine test and would arrange for another nurse to come and do that. She also said that she would prescribe some cream and some stronger pain medication. To date (two days later) no nurse has been to perform the test. The nurse has not prescribed the stronger pain medication as she said, My wife is going to the surgery to try and establish what has happened. Meanwhile, I still am having the same pain, and bypassing the catheter quite a lot. I have been in pain for five days now. This situation has been going on for months with no long term resolution. New catheters, when fitted, stop the pain for a few days, perhaps a week, but the same pain always returns. Whatever is causing the pain has not been resolved. All that happens is I am given something to mask the pain. What I need is an identification of the cause and a cure. The pain is worse today.
Update #5 (5th Aug. '21). It has been six days since my wife first reported my situation. My pain has moved from coming in waves to continual. Today a nurse came to test my urine for an infection. The test was positive. Why has it taken six days for this to happen? Six days of pain. My condition getting worse.It is taking a lot of effort and quite some time to type this. The nurse is going straight to the doctor's surgery to get antibiotics prescribed and to refer me to urology at the hospital urgently. Perhaps now, something will be done to help sort this ongoing issue after eleven months and the current occurrence of almost a week in pain.
Update #6 (6th Aug'21). I have started a course of antibiotics and have a larger morphine patch. The pain has finally gone. I suspect it will return in a week or so but I hope it won't. It has returned in the past to torment me time and time again. When I think it has gone and the future looks brighter, the pain returns after a short break when I am pain free. Then, I have a further problem with my catheter or I contract another UTI or something else happens and the pain is back again. Doctors and nurses typically treat the symptoms and not the cause. I don't think they know what is causing my repeated bouts of pain. A nurse is scheduled today to change my catheter to help with the fight against my latest UTI. I will provide a further update at some future date to explain how things work out.
Update #7 (14th Aug '21) I have been pain free for several days now and my catheter seems to be behaving itself. A few days without pain is a good thing for me. I hope that this continues.

21. Bling. When interacting with a Client, do not wear jewellery. Leave large rings and watches at home for the day; wedding rings are usually OK. Why this rule? Because, during physical interactions I have been ‘caught’ by jewellery many times. Jewellery can have sharp corners and edges which, when brushed against my skin, is painful and likely to evoke a spasm even in a completely different part of the anatomy. For Carers, it is not noticeable unless the Client reacts in pain or starts to spasm in a way that cannot be ignored. Some spasms can be very subtle and, if not watched for, may go unnoticed. A wristwatch brushing against a Client’s skin surely is not a problem, is it? It is! Watches can scratch and cause unwanted Client reactions. The same applies to rings that have gemstones attached. A gemstone is both hard and sharp. Carers’ hands (even while wearing gloves) are in physical contact with Clients a lot of the time. It is likely that rings are going to make contact with skin. If the ring scratches a sensitive area, it can be painful for the Client. Even a necklace may be problematic. A Carer leant over me and her necklace was dangling such that the medallion on the end came in contact with my skin. The medallion was cold. It did not scratch but I am super sensitive to anything cold in contact with the hemiplegic portion of my body. It sent a spasm down my leg and into my left foot. All spasms are uncomfortable and some are painful. A cold medallion, just touching me gently, caused pain. This was unnoticed by the Carers, who carried on regardless. Leave jewellery at home! There is also a chance that Clients, who cannot control movement of hands and arms, could accidentally catch and pull on loose items of clothing or jewellery such as a tie or a necklace. People experiencing learning difficulties may also become attracted by such things and make a grab for them. I stopped wearing a tie after struggling with a person who had taken a firm hold and pulled it and would not let go! I have witnessed staff with long hair in quite some pain while struggling to get free from the grasp of a person who found their hair irresistible.

22. Religion and politics. While it is important that Carers engage the Client in all conversations in an appropriate manner, they should avoid the topics of religion and politics unless the Client initiates a discussion on those areas. Then, listen politely to the person’s views on the matter and, if you disagree, you might steer the conversation gently in a different direction. Do not offend or upset the individual needlessly by arguing or ridiculing any of your Client’s beliefs. If you simply have to talk about either of these things then adopt an exploratory stance by asking your Client,
“What do you think about…?”
“What are your views on…?”
Try to find some common ground from the person’s responses as the area for discussion.
“What do you think about…?”
“What are your views on…?”
Try to find some common ground from the person’s responses as the area for discussion.
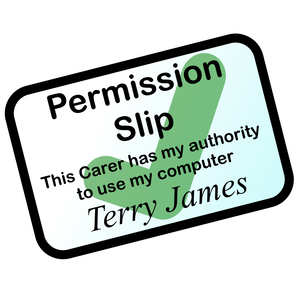
23. Grabbing control. It is not good practice to take a hold of any part of a person without first gaining their permission. Many of the actions you need to perform will necessarily involve physical contact. It is not necessary to seek permission every time for all physical contact involved in a specific task. That is only required until the person understands what is involved in the performance of the task. It may only require explicit explanation for the first couple of times. After that, all that is necessary is to let the Client know what task is about to take place:
“John, we are going to roll you now, OK?”
Never grab a person by any part of their body. Remember the mnemonic ‘paws not claws‘. Use the flat of your hand not your fingertips, which can be very painful especially if you have long fingernails even if you are wearing gloves. Remember, it may be construed as physical abuse if you touch any part of a Client without their permission. Carers will sometimes attempt to pull on my good right arm when rolling me onto my left side. This is not good practice. Pulling an arm, may result in a strain, making the Client’s life a little more uncomfortable. Having to use the right hand only for things, normally achieved using two, places a strain on your fingers, wrist, arm and shoulder after a while. When only one arm is functional, it pays to take good care of it! To experience it for yourself, try going through an entire day without using your left arm and hand for anything at all. Then, imagine having to do that without being ambulant. It is not fun! Do not pull on a Client’s arm. Avoid grabbing and pulling – paws not claws. Never take control without seeking a Client's permission. Never assume Client permission from previous visits, always ask.
“John, we are going to roll you now, OK?”
Never grab a person by any part of their body. Remember the mnemonic ‘paws not claws‘. Use the flat of your hand not your fingertips, which can be very painful especially if you have long fingernails even if you are wearing gloves. Remember, it may be construed as physical abuse if you touch any part of a Client without their permission. Carers will sometimes attempt to pull on my good right arm when rolling me onto my left side. This is not good practice. Pulling an arm, may result in a strain, making the Client’s life a little more uncomfortable. Having to use the right hand only for things, normally achieved using two, places a strain on your fingers, wrist, arm and shoulder after a while. When only one arm is functional, it pays to take good care of it! To experience it for yourself, try going through an entire day without using your left arm and hand for anything at all. Then, imagine having to do that without being ambulant. It is not fun! Do not pull on a Client’s arm. Avoid grabbing and pulling – paws not claws. Never take control without seeking a Client's permission. Never assume Client permission from previous visits, always ask.
24. Leave well alone. Leave the Client’s room as you found it but give the Clients control by asking them questions:
“Would you like me to turn off the light?”;
“Do You want these tissues back on your bed?”
If anything has to be moved, for any reason, ensure it is repositioned prior to leaving the Client. When returning items for a Client, ensure that they are within the Client’s reach and accessible. It is very frustrating to need a tissue, only to discover that, when the Carers put the box back on your bed, they placed them just out of reach and there is nobody at home to help. Remember, just because you would be able to reach an item if you were in the Client’s place, it does not follow that it applies to the Client. I have no use of my left hand and arm.If something is placed on my left side, I have to be able to reach it by using my right hand across my body. I have very poor abdominal muscle control and cannot twist my upper body around. Things that would not be out of reach if I could use my left hand and turn my body, are completely inaccessible to me now, if placed on my left. While it might appear that I ought to be able to reach an object, in my reality, it is not possible.
“Would you like me to turn off the light?”;
“Do You want these tissues back on your bed?”
If anything has to be moved, for any reason, ensure it is repositioned prior to leaving the Client. When returning items for a Client, ensure that they are within the Client’s reach and accessible. It is very frustrating to need a tissue, only to discover that, when the Carers put the box back on your bed, they placed them just out of reach and there is nobody at home to help. Remember, just because you would be able to reach an item if you were in the Client’s place, it does not follow that it applies to the Client. I have no use of my left hand and arm.If something is placed on my left side, I have to be able to reach it by using my right hand across my body. I have very poor abdominal muscle control and cannot twist my upper body around. Things that would not be out of reach if I could use my left hand and turn my body, are completely inaccessible to me now, if placed on my left. While it might appear that I ought to be able to reach an object, in my reality, it is not possible.

25. Smoke screen. Try to refrain from smoking immediately before working with a Client. The Client will be able to smell the smoke on clothes. It is not a pleasant smell. Avoid smoking during the working day if possible. Clients will be able to tell. For a similar reason, avoid wearing strong perfume. While it may seem pleasant to you, it can prove to be quite overpowering for the Client especially when up close by the bedside. The use of a spray-on deodorant for a Client may also be quite overpowering. If in doubt, ask the Client!

26. TV stops work. If a Client is watching something on TV, do not become distracted by it and stop working. See bullet point 4. There is no reason to stop working and stand idle. The Client is likely paying for the service or, at least, somebody is, and your labour is not free. There is no such thing as care without cost; there is always some form of cost to someone somewhere. It is possible to notice what is occurring on TV while providing care, there is no reason to stop working. Chatting, with the Client, about what’s on the TV is good practice. There is no reason to ignore the TV completely. A Carer should never take control and turn off the television or adjust the volume without the Client’s permission. The TV does not prevent work. Although, a loud volume may interfere with some aspects of practice, the Client may have hearing loss and require the additional volume. Refrain from turning down the volume or making any change without the Client’s express permission.

27. Remove glasses. Before rolling, ensure the Client’s glasses are removed. Always ask for permission before removing anything from a Client. Glasses can become an issue and may cause a Client an injury whilst in the act of rolling. If anything has been removed from a Client ensure it is returned immediately on completion of the task. Do not attempt to roll a Client without removing their glasses, if they wear them. It may prove rather uncomfortable if glasses remain in place whilst rolling. There is also a possibility of damage to the glasses. If Carers have removed glasses from a Client for whatever reason, it is their responsibility to ensure that they are back with the Client before they leave. Carers should also check if the Client's glasses require cleaning whenever glasses are returned. Never leave a person on their own without returning their (clean) spectacles. Imagine being alone and virtually blind for hours before the next care visit. Unlikely? Well, it happened to me! Without my glasses, I was virtually blind and could not do anything other than wait until the Carers came for the next visit some four hours later. Why didn’t I tell my Carers that I needed my glasses? It did not occur to me until they had left. Do not not rely on the Client reminding you of a particular need; it is a Carer responsibility.
28. Flesh and bone. When holding a Client to perform an action such as rolling ensure that the person is held by the bony bits of their body, the knee, the hip, the shoulder or the elbow. Never take hold of flesh. The fleshy areas of the body are the most likely to be painful and be hurt. Remember the earlier reference to the use of ‘Paws not Claws’. Claws (fingertips) dig into the flesh and may bruise or leave marks. Paws (flat hands) do not.
Flesh causes stress,
Use bone, alone.
Flesh causes stress,
Use bone, alone.
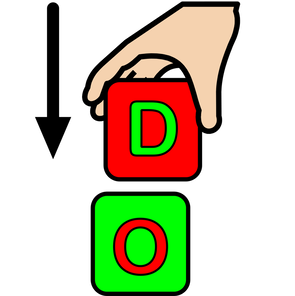
29. If asked – do. If the Client asks for something to be done, then do it immediately unless in the middle of some process for the Client that cannot be stopped. There are not many things that cannot be put on hold until later whilst acting on the Client’s request. It can be very frustrating for a Client to be told, ‘just a second’, ‘in a minute’, ‘just let me do this job’, ‘I’ve only got one pair of hands’, ’when I have done this’, or any other such euphemistic phrase, which usually means the Client will have to wait for much longer and, perhaps, the request never gets fulfilled. Of course, there will be many times when things are very busy and everything just cannot be dropped to perform some action to comply with the request of a Client but, Carers should remain calm and attempt to do that which has been asked as soon as possible. The Client is in control; Carers are there to serve. Do not become stressed, stress can affect the rest of the day and other Clients may suffer as a result. When I was in hospital, I became aware that ‘just a second’ rarely meant a literal second and I could be waiting a very long time. That awareness did not contribute to my recovery one little bit! Try to imagine the Client’s position; s/he probably has realised, whilst lying in a hospital bed, the independence, once taken almost for granted, has forever been snatched away because of some stroke of bad luck (pun intentional). By giving Clients control over their situation, it is helping a little to restore some dignity. That is a worthwhile role!

30. Don’t patronise me. Do not tell a Client to
“Calm down”
if s/he becomes annoyed at some part of your practice (that the Client has been found to be wanting) (Bernstein 2017). Rather, apologise and ask the Client, in a calm manner, to explain what was wrong and to indicate how s/he would prefer the issue to be resolved. Keep a record of the Client’s preferences such that, in future, the routine can be performed to the Client’s specifications. Remember, the goal is control. The Client is ‘in the driving seat’. I was recently told to
“relax”
by a Carer, after the second Carer had sent my left leg and good right arm into spasm by being a little too rough with a particularly sensitive part of my anatomy. When I pointed out that the remark was unprofessional, the Carer informed me the second Carer was new and did not know about my situation. That was no excuse for unprofessional behaviour. Always pair new Carers with one having experience such that the latter is able to advise, educate and guide the novice appropriately. All Carers should read the Client Care Plan before attending a Client.
“Calm down”
if s/he becomes annoyed at some part of your practice (that the Client has been found to be wanting) (Bernstein 2017). Rather, apologise and ask the Client, in a calm manner, to explain what was wrong and to indicate how s/he would prefer the issue to be resolved. Keep a record of the Client’s preferences such that, in future, the routine can be performed to the Client’s specifications. Remember, the goal is control. The Client is ‘in the driving seat’. I was recently told to
“relax”
by a Carer, after the second Carer had sent my left leg and good right arm into spasm by being a little too rough with a particularly sensitive part of my anatomy. When I pointed out that the remark was unprofessional, the Carer informed me the second Carer was new and did not know about my situation. That was no excuse for unprofessional behaviour. Always pair new Carers with one having experience such that the latter is able to advise, educate and guide the novice appropriately. All Carers should read the Client Care Plan before attending a Client.

31. Don’t look back in anger. If a Client is being difficult, do not aggravate the situation further by making a facetious comment such as,
“who got out of the bed on the wrong side this morning?”
Ask the person to try to explain what is upsetting him / her. Let the Client know that Carers are willing to help. The Client should come to understand that everything, within your power, would be done to resolve the issue. Clients should trust Carers and feel safe in their care, welcoming their arrival throughout the day. Returning a Client’s anger will only make a difficult situation worse and can affect future visits negatively. Remain calm and let the Client know that s/he is in charge and Carers are there to help.
“who got out of the bed on the wrong side this morning?”
Ask the person to try to explain what is upsetting him / her. Let the Client know that Carers are willing to help. The Client should come to understand that everything, within your power, would be done to resolve the issue. Clients should trust Carers and feel safe in their care, welcoming their arrival throughout the day. Returning a Client’s anger will only make a difficult situation worse and can affect future visits negatively. Remain calm and let the Client know that s/he is in charge and Carers are there to help.

32. I swear I didn’t. It is very unprofessional to use profanities in the presence of a Client. Even if a Client is using vulgar language whilst communicating, do not be tempted to reciprocate. Maintain your professionalism. The 'f-word' has been used several times by Carers and other ripe language is not uncommon. I am not offended, I have heard cursing all of my life. I have even used it myself on occasion. There is a place for bad language and it definitely isn't while with a Client. It is not professional, leave it in the street.
 Click to enlarge.
Click to enlarge.
33. Punctuality is timely. Presumably, attendance to provide care for a Client is at established times throughout the day. It is good practice to inform the Client if there has been a delay and the team’s arrival is going to be late. I have been expecting support to arrive, at a specific time, only to be kept waiting for long periods not knowing what has happened or if I am going to get the care, for which I pay, at all. There have been many occasions on which Carers have failed to arrive at the usual time and I have not been informed. Having to wait for long periods, perhaps in pain, for a service and the team have not even bothered to inform the Client that they are running late, is not something about which anyone would be very happy. Even worse, if the Carers do not turn up at all!
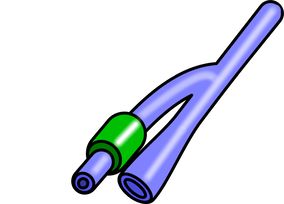
34. Go with the flow. If the Client has a catheter, double-check the night bag. Is the night bag properly attached to the leg bag? Is the leg bag’s valve in the open position such that urine can flow freely from the leg bag? A leg bag alone may not have sufficient capacity to handle the volume of urine passed during the night. A leg bag, full to capacity, will prevent the Client’s bladder from emptying and may cause serious pain (Herter, & Kazer 2010)

35. Don’t strain yourself. If the Client watches TV or has a monitor for any other purpose, ensure s/he has an unobstructed view of it before leaving. Position the Client’s bed such that the screen can be viewed without having to strain. The Client should be able to see the monitor whilst in a comfortable and natural position. Ensure that your Client has access to all the gadgets s/he requires to be in control. The remote for the TV should be in easy reach, for example. I am frustrated when items that I may need are placed just slightly out of my reach. I will strain to reach them, often failing, as a little more than half of my body is not functioning correctly. Carers assume that I am able to move my body a little to be able to reach for nearby items. I cannot do that. My abdominal musculature is not functioning well since the stroke and I have very limited movement.
36. Naked and cold. The Client may prefer to be naked while in bed and may not wear any bedclothes. When the covers are removed, the covers that were keeping your Client warm, remember s/he is now exposed the elements and may start feeling Cold. While Carers might be quite warm, fully dressed and active, the Client might be having a quite different experience. Try to imagine being naked in a room in the presence of strangers tasked in a caring role; what should happen? Feeling exposed and embarrassed would be natural. Within a short time, it is also normal to feel cold. What should occur? Perhaps Carers could temporarily cover up parts that may be embarrassing and get on with the job efficiently such that the Client can be back under his / her blankets as soon as possible. A person should not be naked for longer than is absolutely necessary. Always ask the Client,
"Are you warm enough? Please say if you start to feel chilly"
"Are you warm enough? Please say if you start to feel chilly"

37.Come in from the cold. Some Clients with disabilities may be super sensitive in specific areas of their body. A paralysed limb resulting from a stroke, for example, may not be immune to sensations. In fact, the limb may be super sensitive. If cold hands come into contact with such a limb, it may be felt like an electric shock resulting in painful spasms in several areas of the Client’s anatomy. Simply forewarning (and apologising to) the Client that your hands are cold and then proceeding to touch the Client’s body anyway is very poor practice. Always warm your hands. There is usually a sink and hot water available for this purpose.

38. Wash and dry. When washing a Client, ensure that it is done properly. Ensure that whole limbs or any parts, requiring daily cleaning, are not missed (Burns, & Day 2012; Lawton, & Shepherd 2019). After washing, ensure the Client is dried properly. Carers will probably be wearing some form of rubber or plastic protective gloves whilst with a Client. In which case, it will be more difficult to tell, by touch, whether a specific area of the Client’s anatomy is completely dry. Always ask the Client if s/he feels dry. Ask, also, about deodorant and talcum powder, do not just assume or completely forget. Isn’t all this just common sense? Not so! I have experienced a daily ‘wash’ for almost a year and the difference in standard between the arriving Carers is huge.
First Carer: “Do we wash with any soap?”
Second Carer: “Oh, don’t bother with that, just use plain water.”
Common sense? It obviously is not ‘common’ as not all have the same basic level of practice. Neither is it ‘sense’ because, if it was, it would be natural and all would do it, at least in a basic manner. This morning, one of my Carers appeared as though she had a stroke herself resulting in a right side neglect. She only washed the left side of my right leg and the left side of my chest! I, long ago, gave up trying to tell Carers about washing; they either become very defensive, angry, or claim they were going to do it anyway and state,
“You must be more patient”.
The reward for my ‘patience’ is typically a wash that is more like a quick wipe. I very rarely receive a good wash; Carers wipe some areas of my body and neglect others. I calculate that Carers have only washed the left side of my abdomen four times in the last nine months. When Carers roll me on to my right side, they have access to my left side but they usually neglect washing this area. I used to bathe every day before I had the stroke. I cannot have a bath now because there is no way of getting me upstairs, no means of getting me into the bath and, no means of preventing me from slipping under the water and drowning whilst in the bath! Nearly a year without a shower or a bath. How would you feel? Now add to that, washes that are mostly inadequate. I am going to suggest that, one day a week is ‘good wash day’. On this day, the Carers would have to take more time to wash me thoroughly. Carers often do not wash my groin properly if at all. I suppose some Carers are embarrassed to go ‘down there’. However, it is one area requiring special attention. It often becomes sore and painful due, I suspect, in some measure, to a lack of personal hygiene.
Wearing gloves reduces sensory feedback and Carers need to pay particular attention to temperature and dryness. I have had my hair washed with water that is too cold or too hot. It is very important that Carers ask the Client about temperature with a small test sample before committing to the full wash. Likewise with dryness, don't be too vigorous, proceed gently and ask the Client if s/he feels dry.
I am super-sensitive since the stroke. When I am washed, the flannel feels coarse on my skin. It is as though I am being rubbed with wire wool. Towels that used to feel soft and fluffy now appear harsh and scratchy. I don't feel clean after a wash, I feel scraped. On areas that are sore, use a very light touch. Drying a slightly sore area with a towel normally is very likely to make that area sorer. Be especially gentle and use a delicate touch with the towel. After I have been washed and before I am dried with a towel, the water on my skin starts to evaporate off and makes that area appear especially cold. It lasts until I am dried with a towel. Carers should ensure they dry an area as soon as possible after it has been washed and not leave it while they wash another area. All Carers should experience the sensation themselves. Get a spouse or partner to wash your body while naked in bed. Pretend to be unable to move and get something of the 'disability experience'.
Wash and dry,
Don't pass by.
Soft towels appear rough,
So don't be too tough.
Don't pass by.
Soft towels appear rough,
So don't be too tough.
39. A pain in the bum. It is common for people, remaining motionless in bed for long periods, to develop bedsores. Bedsores are incredibly painful. Cleaning the skin of my bottom several times a day with wet wipes does not help. This only tends to make the skin sore. The skin on a person’s bottom requires a gentle touch. At the first sign of soreness, the nursing service should be informed. I have found that some creams, used to prevent further infection, sting so badly that I refuse to let anyone apply them. Sitting in urine or faeces, for any length of time, without immediate cleaning, can compound the situation. Seek medical advice as soon as the first signs of any soreness appear. Notify Significant Others of the concern. Never pull through a sheet or anything that could cause friction (even slide sheets cause friction) between the skin of the bottom and the surface of the item removed. While it may be believed the item is smooth (for example, a bed sheet) and unlikely to cause any problems, believe me, it is felt by the Client as it is pulled through under his / her body, and it can be very painful especially to an already sore posterior, and may break the skin. The sling, used in hoisting, is especially problematic in this area. It is not smooth and, with incorrect use, the resulting friction burns can cause excessive pain. I have an ongoing problem with pressure sores. ‘Pressure sores’, ‘bed sores’, or ‘pressure ulcers’ (variant names for the same condition) are damage to the skin and underlying tissue, caused by a sustained pressure on the skin due to the weight of a body over time. People that are unable to change position in bed or in a chair readily are especially vulnerable. Sustained pressure on an area of the skin can impair the blood supply, which can lead to the condition. Sores are painful things especially as the Client has to lie / sit down on them again. Carers should be very gentle in cleaning areas containing a sore. This morning, the Carers cleaned my bottom with a wet-wipe as is normal. It was very painful. Wet-wipes can feel very harsh on sensitive skin especially with repeated wiping. As moisture on the skin can increase the risk of developing pressure sores, areas that are washed, or cleaned with a wet-wipe, should be thoroughly but gently dried afterwards. Clients with a pressure sore should not be in a seat for more than 2 hours without some form of repositioning (DeFloor and Grypdonck, 1999). If the Client exceeds this time, return the Client to bed, with suitable pressure management, for no less than 1 hour (Gebhardt and Bliss, 1994; Defloor and Grypdonck, 1999). Thus, if a Client (sitting in a chair) is indicating that his / her bottom hurts, take it seriously and make every effort to reposition the Client and, if possible, return the Client to bed. I have found that, hoisting slings can contribute towards becoming uncomfortable. Remove the sling, immediately after use, if possible, should a client be likely to remain in a single seated position for more than twenty minutes. If the client already has a pressure sore, this is true for ‘stay in place’ slings as well. Additional products to help with the management of pressure sores (beyond those that the NHS is able to supply) can be beneficial (Cullum et al, 2000; McInnes and National Institute for Clinical Excellence, 2004). However, there is no clear evidence, which are the best products to use in the effective management of sores (McInnes and National Institute for Clinical Excellence, 2004). If a Client has a sore or anything that might possibly develop into a sore, contact the nursing services immediately. Do not assume that someone else is sure to do it, ensure that someone will. On a following call, check that the matter is now with the nursing service and that, at least, weekly monitoring is in place. Do not attempt to treat the sore yourself, unless medically qualified to do so, always seek medical advice from the local nursing provision. The nurses will treat and maintain a record of the sore, ensuring that it will not become worse. They are likely to dress an open wound. A dressed area should be treated carefully. A dressing should not be removed by other than the nursing team managing the situation, without their express permission, even if soiled. Rather, report observations immediately to the proper authority. Effective management and debridement of stores is the key to returning a Client to better health and reducing the risk of the sore developing into a greater danger (Romanelli and Mastronicola, 2002; Cutting and White, 2004). Details of Pressure sore practice should be in the Client’s Care Plan.

40. A weighty matter. Often, when Carers are performing some routine function they may need to reach across a Client’s body in order to achieve a particular task. In doing so, they may rest an arm or hand on the Client’s bed directly above a Client’s body. While it may appear, to a Carer, that this is an innocent action, the Client may have very sensitive body areas and the action maybe causing the Client undue problems. This is especially true for Clients who have had a stroke, for example (Boivie 2006; Akyuz & Kuru 2016; Nagasaka, Takashima et al 2017). Stimulation of one sensitive part of their body can set up a chain reaction leading to painful spasms in another area. Furthermore, although it may not be realised, even a slight pressure can feel very weighty to a Client and be very uncomfortable. Avoid resting any part of your body on any part of the bed currently occupied by your Client.
41. Baby, it’s cold outside. Following the time I spent in hospital, I have had care, at first, for four times a day and later, I cut it to three times daily. That is, at least, one thousand care calls. Each visit, the Carers have to reposition me in the bed and that requires the use of a slide sheet. On almost every occasion, the Carers warn me, as they roll me off my side and onto my back on the slide sheet,
“it’s going to feel cold, sorry.”
My room is at a constant temperature, it never varies and the slide sheet stays near to my bed, in my room. As such, the slide sheet must be at room temperature. It cannot go below. After a thousand visits, I know how the slide sheet is going to feel, I do not need repeatedly to be informed of its temperature! It would drive me crazy if I did not find it amusing! The things Carers say!
“it’s going to feel cold, sorry.”
My room is at a constant temperature, it never varies and the slide sheet stays near to my bed, in my room. As such, the slide sheet must be at room temperature. It cannot go below. After a thousand visits, I know how the slide sheet is going to feel, I do not need repeatedly to be informed of its temperature! It would drive me crazy if I did not find it amusing! The things Carers say!
42. Remarkable.
“I left my children to come and help you and
I am worried about them.”
This was said to me by a Carer (in an angry tone of voice). I had done nothing to provoke such an outburst and I thought the remark unprofessional.
“Angry people are not always wise.”
(Jane Austen, Pride and Prejudice, first published January 28th, 1813)
I was paying for the service and, thus, for her time. If that person did not want the job, she need not have taken it. I understand that she probably needed the income and, yet, had to leave her children sometimes when she had to work but her wrath was misplaced directed at me. Do not take out personal frustrations on a Client. Leave them at home. The remark was a little upsetting and did not help me at all. What is said is as important as what is done!
“I left my children to come and help you and
I am worried about them.”
This was said to me by a Carer (in an angry tone of voice). I had done nothing to provoke such an outburst and I thought the remark unprofessional.
“Angry people are not always wise.”
(Jane Austen, Pride and Prejudice, first published January 28th, 1813)
I was paying for the service and, thus, for her time. If that person did not want the job, she need not have taken it. I understand that she probably needed the income and, yet, had to leave her children sometimes when she had to work but her wrath was misplaced directed at me. Do not take out personal frustrations on a Client. Leave them at home. The remark was a little upsetting and did not help me at all. What is said is as important as what is done!

43. Do not forget me. Elderly Clients and others experiencing learning difficulties may have problems with remembering names (Yoon, Ooi et al 2018). If you are attending such a Client always begin the session by introducing yourself:
“Good morning John, it’s Helen, your Carer, come for your morning call. How are you today?”
It is a good idea to get into the habit of introducing yourself as you enter the Client’s room such that it becomes a habit and occurs without thinking.
“Good morning John, it’s Helen, your Carer, come for your morning call. How are you today?”
It is a good idea to get into the habit of introducing yourself as you enter the Client’s room such that it becomes a habit and occurs without thinking.
44. Plots and plans. Each Client must have a Client-Centred Care-Plan (CCCP) (McLoughlin, Bayati-Bojakhi et al 2014) that is accessible for Carers to read prior to the provision of support. The plan should be amendable only via a specified route safeguarding the Client. The plan should include such things as Client condition, preferences, dislikes, potential areas of concern, specific practice to avoid, communication methodology, medical issues, advocates, family information, menu plans, hygiene practice, contact details, health and safety, and any other pertinent information that Carers might require to be able to provide the best professional person-centred service possible. No person providing care should attend a Client ‘blind’, that is, without knowing anything about the Client and her/his condition and needs. If staff absence (or other unforeseen events) mean that a novice must be utilised, always pair with a Carer that has experience with the Client and is familiar with the routine. One day, two Carers arrived who had never been on a morning visit with me. They admitted they did not have any experience and did not know what to do. I informed them that there should be a Care Plan. Their response?
“We haven’t read it. You don’t think that we have the time to read every person’s Care Plan, do you?”
During the 30-minute session, they made nine basic errors (points outlined on this Web page ). After they left, I had my blood pressure taken; it was ten points higher than normal. It defeats the objective of ‘care’ if the very act of caring makes the Client ‘sicker’ than before the ‘caring session’.
Health Warning: Poor quality care may be harmful to healthy living!
“We haven’t read it. You don’t think that we have the time to read every person’s Care Plan, do you?”
During the 30-minute session, they made nine basic errors (points outlined on this Web page ). After they left, I had my blood pressure taken; it was ten points higher than normal. It defeats the objective of ‘care’ if the very act of caring makes the Client ‘sicker’ than before the ‘caring session’.
Health Warning: Poor quality care may be harmful to healthy living!
45. Location, location. In verbal and physical interactions with the Client try to ensure positioning such that the Client can see everyone clearly, and preferably make eye contact. To perform some form of physical manipulation of a Client when the Carer is located in a position, behind the person, out of sight and, without a verbal warning, could be construed as a form of physical abuse (Adigun, Mikhail et al 2020). Let the Client see and hear what you are going to do such that s/he can prepare for the forthcoming action. Never take hold of any part of a person’s body without forewarning the person of your intention. It is OK if the action itself necessarily involves repeated physical contact, just explaining what is about to happen without asking permission for every physical contact you will need to make. Although, the first couple of times that the Carers perform the action, it may be necessary to go into the details of each step involved seeking permission. When the Client has become accustomed to the process and knows what to expect, then it is enough to announce the particular action,
“John, we are going to roll you onto your left side, OK?”
and wait for the Client to respond in the affirmative before proceeding.
“John, we are going to roll you onto your left side, OK?”
and wait for the Client to respond in the affirmative before proceeding.

46. Hand in hand. There may be times when it proves necessary to help a Client by gently taking their hand and moving it to assist in the performance of a specific action. The normal way this is undertaken is with a hand over hand approach. The Carer’s hand takes the Client’s hand and guides it to accomplish the task. Why is this the wrong approach? What does the Client see? Because the Carer’s hand is over the Client’s, they see the Carer performing the action! Better, if the Carer adopts a hand under hand approach such that Clients see their hand moving to achieve the task with the Carer’s hand underneath supporting and guiding the process. Hand under hand is the preferred method.
47. Danger full! People that are fitted with a catheter generally require a night bag attaching in addition to their leg bag to allow extra capacity during the hours while the person is asleep. The leg bag alone would not have enough capacity to allow for the collection of urine during the period between the last call of one day and the first call of the next. A full catheter bag would not allow urine to flow from the bladder and could cause a Client significant distress. It is for this reason that it is very important to remember to check that the valve from the leg bag to the night bag is fully open such that urine is able to flow freely from one to the other. There are several different types of valve utilised by leg bags and, therefore, it is easy to make a mistake and not open the valve fully, especially with a valve that, previously, has not been encountered. A useful tip for this situation is to leave a small amount of urine in the leg bag from the previous call to test that the valve is properly opened after the night bag has been attached. Does the urine flow out of the leg bag? Does the leg bag empty? If the answer to these questions is yes, then the Carer can be assured that the valve is opened to the correct position and the Client is not likely to have trouble from it during the night. Remember to check that the night bag is properly attached and the valve is fully open.
48. The leg bag’s connected to… The night bag's connected to the leg bag.The leg bag's connected to the catheter. The catheter's connected to the genitalia. The genitalia's connected to the bladder. The bladder's connected to the kidneys. Now hear the word of the... As the song almost goes!
Catheters usually travel via the Client’s genitals to the bladder. It is not a good idea to pull on the tube therefore, as this is likely to cause the Client a lot of pain. It is important, when changing a leg bag, or adding a night bag, to ensure that care is taken to avoid tugging on the catheter. This equally applies when doing anything that might involve movement of attachments to a catheter (for example, when rolling, hoisting, or repositioning). Be catheter aware!
49. Losing it. Occasionally, it will be necessary to work with a Client who is displaying behaviour that people may find challenging. (Kneebone & Lincoln 2012; Alderman 2013; Andrewes, Walker, & O’Neill 2014;) Challenging behaviour might occur any point during a call or the Client may exhibit such behaviour throughout. At times, being disabled can be frustrating and it is hardly surprising for POD to have the occasional outburst. Do not take it personally, probably the anger is directed more at the situation than at any one person. It is important to note that usually behaviour found to be challenging is not simply a part of the person’s character but typically has a specific trigger. The triggering event may not have been due to an issue with a particular Carer. It may be rooted in some previous experience with other Carers (even with Carers from long ago). The Client having generalised it to all Carers that come to call. If a person suddenly starts to exhibit behaviour that anyone would find challenging during your call, ensure a record is made of the events detailing A B C. Where A is for Antecedent; what was happening prior to the behaviour occurring? What were you doing? B is for Behaviour; what form did the behaviour take? Try to describe the behaviour factually without using pejorative or judgemental terminology such as ‘bad’, ‘terrible’, ‘unprovoked’. C is for Consequences; what happened because of the person’s behaviour? Did the behaviour stop suddenly? Did the response to the behaviour have an effect? At some later and calmer time, away from the Client, go through the ABC(s) and try to establish a possible triggering event. What did you do in response to the behaviour? Was it successful? Did it bring calm and restore peace or did it make no difference or make matters worse? Consider what might have been done differently, both before, so as not to trigger the behaviour, and after, to restore calm? For example, if it is discovered that the challenging behaviour has always occurred following rolling, it is reasonable to suspect that something occurring during this procedure is a trigger for the behaviour. I, regularly, am in pain when I am rolled onto my side because carers have a habit of pushing their fingertips into my flesh in order to gain a better hold to be able to move me or into the flesh of my inner thigh to pull my legs apart (particularly painful). The flesh on my legs and my sides is very sensitive and the action causes a lot of pain. I could elect to react with an outburst of anger but I choose to ignore it these days, as it only lasts briefly, and they release their grip as soon as they accomplish their task. I have shouted at Carers previously when their fingertips caused me pain but my reaction only elicited irate excuses, from the Carer, about having to hold me firmly in order to roll me. Responding to behaviour that people find challenging with anger can only serve to make a bad situation worse. Carers should do all that they can to prevent such an outcome. While I should not have shouted at my pain, the Carers should not have reacted as they did. They should have remained calm, listened to my complaint, apologised and changed their practice in future. On reflection, ask, if your response acted to calm or Inflame the situation? If the latter, consider an alternative course of action, one in which the situation remains calm and has a positive outcome. Do not be tempted to suggest that the Client should,
“calm down”, “pull yourself together”
or some other such remark. Is there another person available whom might provide assistance? Do not allow the situation to escalate further. Are the Carers aware of a Client’s BEST? (Best Ever Stimulating Things). BEST is the particular thing (or things) the Client likes. For example, a specific song or style of music, a favourite event / period from the past, a preferred object, place to be, a treasured photograph or picture. Would the provision of any BEST restore some tranquillity? If so, ensure it is available and easily accessible to use in any future similar occurrence. Prevention is better than cure; try to avoid any triggering events in all future interactions. It may be the consequences of a particular behaviour prove to be rewarding for the Client. S/he might like the level of attention that results from a behaviour and the attention is reinforcing the behaviour. As such, the behaviour found to be challenging is more likely to occur in the future. In this instance, it will be necessary to refrain from providing the rewarding response and search for an alternative. It may not be the response to the challenging behaviour as such that the Client finds rewarding but, rather, the individual providing the response. Your Client may really like having that particular person’s attention. Changing the outcome perhaps changes the behaviour. Try using a different person to act in response to the behaviour. Challenging behaviour can be quite difficult to analyse and rectify. A team of people best addresses it with access to professional advice. However, there are some simple items for the TREATMENT of the Client which should be put into practice to help lessen the frequency with which behaviour that people might find challenging occurs:
“calm down”, “pull yourself together”
or some other such remark. Is there another person available whom might provide assistance? Do not allow the situation to escalate further. Are the Carers aware of a Client’s BEST? (Best Ever Stimulating Things). BEST is the particular thing (or things) the Client likes. For example, a specific song or style of music, a favourite event / period from the past, a preferred object, place to be, a treasured photograph or picture. Would the provision of any BEST restore some tranquillity? If so, ensure it is available and easily accessible to use in any future similar occurrence. Prevention is better than cure; try to avoid any triggering events in all future interactions. It may be the consequences of a particular behaviour prove to be rewarding for the Client. S/he might like the level of attention that results from a behaviour and the attention is reinforcing the behaviour. As such, the behaviour found to be challenging is more likely to occur in the future. In this instance, it will be necessary to refrain from providing the rewarding response and search for an alternative. It may not be the response to the challenging behaviour as such that the Client finds rewarding but, rather, the individual providing the response. Your Client may really like having that particular person’s attention. Changing the outcome perhaps changes the behaviour. Try using a different person to act in response to the behaviour. Challenging behaviour can be quite difficult to analyse and rectify. A team of people best addresses it with access to professional advice. However, there are some simple items for the TREATMENT of the Client which should be put into practice to help lessen the frequency with which behaviour that people might find challenging occurs:
- Treat the Client as an adult at all times,
- Remain calm and professional throughout the session,
- Ensure that the Client is in control,
- Ask for permission before making changes, leave the environment Alone,
- Talk with the Client, Don’t swear, Be polite,
- Maintain peace & calm, Keep opinions to yourself unless asked,
- Enter on time, consistently,
- No use of fingertips; paws not claws,
- Talk to the Client using given first name.

50. Coughs and sneezes spread diseases
https://www.youtube.com/watch?v=W728NGYhmmQ
If a Carer has a cold, s/he should not be around vulnerable Clients. The Client already has enough problems with which to deal; s/he will not thank you for an additional one. If Carers are relatively healthy, and find having a cold troublesome, image what that cold would be like to a person with disabilities. Cold today? Stay away! Carers should keep germs to themselves. Ask for other duties if possible; do not put vulnerable Clients at risk. At the very least, wear a mask and ensure that your hands are clean. Attempt to keep physical interactions with your Client to a minimum.
https://www.youtube.com/watch?v=W728NGYhmmQ
If a Carer has a cold, s/he should not be around vulnerable Clients. The Client already has enough problems with which to deal; s/he will not thank you for an additional one. If Carers are relatively healthy, and find having a cold troublesome, image what that cold would be like to a person with disabilities. Cold today? Stay away! Carers should keep germs to themselves. Ask for other duties if possible; do not put vulnerable Clients at risk. At the very least, wear a mask and ensure that your hands are clean. Attempt to keep physical interactions with your Client to a minimum.

51. Rocking and a rolling. (Vatwani 2017) It takes time for a Client to feel safe when being rolled. The Client ends up on his / her side on the edge of the bed and can feel insecure. Carers should reassure the Client of their safety and are very unlikely to fall. A further problem encountered when rolling Clients is dizziness. When rolled too quickly, I felt as though my room had begun spinning. It had made me feel somewhat sick for a while, after the Carers had left, until my vision had returned to normal. Roll slowly and carefully. Rolling is not a pleasant procedure for the Client. It Can result in dizziness, upset stomach, spasms, and pain. The best practice is to ensure that rolling is done gently and kept to a minimum. In one visit I had to be rolled ten times due to positioning and other errors by the Carers.

52. Bloody café. While in hospital, I had been moved into a room just off the main stroke ward. I grew to hate being in a room on my own because, once the door is shut, you really are on your own. As an IRON POD, being isolated in hospital is frightening. Sure, there is a nurse call button to summon assistance but it has to be in reach otherwise it may as well not be there. I got used to the nurse call button taking many minutes to summon a nurse (on one occasion, it took 45 minutes before my call was answered). It scared me somewhat to know that I was completely dependent on others and, yet, I had no means of calling for those ‘others’ in an emergency. I might be choking and press the nurse call button and be dead before anyone answered my call. Thankfully, that scenario never happened but it frightened me nevertheless. One night, around one in the morning, I really needed a drink. I pushed the nurse call button and waited. Nearly twenty minutes later two nurses came into my room. I asked for an orange juice from the fridge (my wife brought me cartons of juice, which she put in the fridge in the nurse’s office to keep them cool and fresh on the advice of day staff). One nurse looked sternly at me and said,
“Do you think this is a bloody café”?
However, I did get my juice but, such incidents, made me wary of calling for help during the night at all. I reported the incident to my wife when she came to visit. She informed the PET (Patient Experience Team) section of the hospital but, as far as I am aware, nothing much happened. The leader of the night staff did call my wife and said such behaviour was unacceptable. He said that he would talk to his team to ensure better practice but no nurse ever apologised and things did not improve. There were further incidents some of which, I have already reported at the beginning of this paper. Hospitals should not be frightening places. As an IRON POD, I dread having to go back there.
“Do you think this is a bloody café”?
However, I did get my juice but, such incidents, made me wary of calling for help during the night at all. I reported the incident to my wife when she came to visit. She informed the PET (Patient Experience Team) section of the hospital but, as far as I am aware, nothing much happened. The leader of the night staff did call my wife and said such behaviour was unacceptable. He said that he would talk to his team to ensure better practice but no nurse ever apologised and things did not improve. There were further incidents some of which, I have already reported at the beginning of this paper. Hospitals should not be frightening places. As an IRON POD, I dread having to go back there.
53. There’s nothing worse. Carers come for three calls a day. I often am in some form of distress. Carers ask
“what’s wrong?”
and I try to reply, if I am able to speak at all depending on the intensity of the pain at that time, to inform them of the issue. It might be bowels, catheter, earache, toothache, leg spasms, arm aching, headache, I’ve had them all over the months since my stroke. Whatever I state as the cause of my pain, the usual response is:
“There’s nothing worse.”
“Headache? There’s nothing worse.”
“Toothache? There’s nothing worse.”
“Constipation? There’s nothing worse.”
“Earache? There’s nothing worse.”
And so on. By definition, there can only ever be one solitary worst condition. Stating, as fact,
“There’s nothing worse”
to me, in bed, paralysed down the left hand side of my body, makes me want to shout out loud,
“being paralysed down the left hand side of my body, and confined to bed virtually 24/7, in pain a lot of the time."
Guess what? -
"There’s nothing worse!!!”
You have to laugh (Don’t you?).
“what’s wrong?”
and I try to reply, if I am able to speak at all depending on the intensity of the pain at that time, to inform them of the issue. It might be bowels, catheter, earache, toothache, leg spasms, arm aching, headache, I’ve had them all over the months since my stroke. Whatever I state as the cause of my pain, the usual response is:
“There’s nothing worse.”
“Headache? There’s nothing worse.”
“Toothache? There’s nothing worse.”
“Constipation? There’s nothing worse.”
“Earache? There’s nothing worse.”
And so on. By definition, there can only ever be one solitary worst condition. Stating, as fact,
“There’s nothing worse”
to me, in bed, paralysed down the left hand side of my body, makes me want to shout out loud,
“being paralysed down the left hand side of my body, and confined to bed virtually 24/7, in pain a lot of the time."
Guess what? -
"There’s nothing worse!!!”
You have to laugh (Don’t you?).

54. Keep informed. If there is an issue with anything to do with a Client, do not keep it to yourself, inform a significant other: a therapist, a spouse or other family member, call for medical assistance, talk to your team leader, involve social services… If uncertain as to what to do, ask a senior member of staff for advice, do not put it off, believing someone else is sure to deal with the problem. If someone has been told and the situation remains the same, inform another of your concerns. Do not allow a little problem to become an emergency (Health and Care Professions Council 2015).
55. Check it. It is good practice to have a checklist for specific events during a visit (Wolff, Taylor, & McCabe 2004; Gawande 2009). For example; for use when rolling:
- Bone not flesh
- Paws not claws
- Glasses 👓?
- Tell before do
- Roll left is preferred
- Cannot maintain right side position, requires assistance
- …
Choice Is A Voice
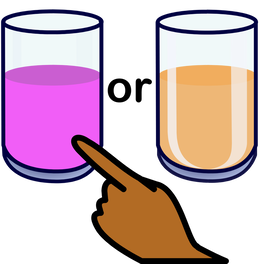
56. Choice is a voice. Always give the Client a choice (Dixon, Robertson et al 2010; Mulley, Trimble, & Elwyn 2012) but don’t constrain the Client to choices that Carers find acceptable: don’t ask,
“would you like tea or coffee?”
rather ask
”would you like tea or coffee or something else?”.
In this way, the Client is permitted a freedom to choose any drink at all. While in hospital, I was asked what I would like for breakfast, and had a good choice, as many options for breakfast are, by coincidence, often vegan. However, institutional meal choice for vegans is typically very poor, something of a Hobson’s choice – take it or leave it. For example, while vegan Alpro yoghurt was an option on the menu, there was only one flavour; thus, no real choice. Hobson’s choice isn’t really a choice at all. It is, rather, a single option only. The phrase is said to have originated with Thomas Hobson (1544 – 1631), a livery stable owner in Cambridge, England, who offered customers the choice of either taking the horse in the stall nearest to the door or taking none at all. Providing real choice is another way of passing control of the situation to the Client. After days of no or poor choice, my wife had to bring in my main meal each day (at visiting time) which she cooked at home and kept, at least, vaguely warm by wrapping each Tupperware box, containing meal courses, in towels during the journey to my bedside. In this way, I was able to choose what I wanted to eat for my main meal on the next day and be assured it would be vegan. The goal is control. Choice is a voice.
“would you like tea or coffee?”
rather ask
”would you like tea or coffee or something else?”.
In this way, the Client is permitted a freedom to choose any drink at all. While in hospital, I was asked what I would like for breakfast, and had a good choice, as many options for breakfast are, by coincidence, often vegan. However, institutional meal choice for vegans is typically very poor, something of a Hobson’s choice – take it or leave it. For example, while vegan Alpro yoghurt was an option on the menu, there was only one flavour; thus, no real choice. Hobson’s choice isn’t really a choice at all. It is, rather, a single option only. The phrase is said to have originated with Thomas Hobson (1544 – 1631), a livery stable owner in Cambridge, England, who offered customers the choice of either taking the horse in the stall nearest to the door or taking none at all. Providing real choice is another way of passing control of the situation to the Client. After days of no or poor choice, my wife had to bring in my main meal each day (at visiting time) which she cooked at home and kept, at least, vaguely warm by wrapping each Tupperware box, containing meal courses, in towels during the journey to my bedside. In this way, I was able to choose what I wanted to eat for my main meal on the next day and be assured it would be vegan. The goal is control. Choice is a voice.
"The starting point is not a test of capacity, but the presumption that every human being is communicating all the time and that this communication will include preferences. Preferences can be built up into expressions of choice and these into formal decisions. From this perspective, where someone lands on a continuum of capacity is not half as important as the amount and type of support they get to build preferences into choices."
Beamer and Brookes (2001, page 4)
Making a decision involves having a choice. However, having a choice and decision-making cannot be viewed simply in one way; there is in fact a 'Continuum of Choice'.
The continuum may be split into four areas:
- Independent Choice (Contained and Complete);
- Supported Choice;
- Substitute Choice;
- Hobson's Choice (No Choice);
Independent decision-making involves the Client deciding for herself / himself without the assistance of any outside person. Even if the Client were to ask another's opinion, any decision reached would still be considered as independent.
- Contained Choice is defined as a choice that is governed by some external limiting factor imposed by another. Examples of Contained Choice include the provision (by an another) of an array of items from which a Client may select: for example, apple juice or orange juice when a drink is required. The choice is 'contained' to one of two options decided by and thus constrained by another person.
- Complete Choice is defined as a complete freedom of choice. Although circumstances themselves may act to constrain the choice. While many would consider this notion chimeric, an important factor in reports on quality of life issues is the amount of control an individual is able to exert over daily events and his/her ability to makes choices.
One may argue that the notion of Complete Choice is an illusion and that all choice involves some aspect of constraint:
" Human beings are essentially social creatures. What they are and what they might be depends both on themselves and upon the societies in which they grow up and make their choices. Choices, however, are always made within some framework of constraint."
(Twine 1994)
but, as choice becomes increasingly controlled by outside agencies so quality of life is reduced to the point where the individual becomes a puppet or a slave acting only on the permissions of another.
While both contained and complete choices may have consequences, typically, Significant Others support contained choices by removing those that may have detrimental long term effects. Although some individuals may be able to make an everyday contained choice independently (tea or coffee?), they might need significant assistance with complete choices that have far longer term consequences (Live at home or live in sheltered provision in the community?).
It should be noted that, at different times and in different situations, Clients may be independent in one area of choice and supported in another and 'experience' (in a sense the Client does not experience as another makes the choice on his/her behalf) substituted choice at others.
Supported decision-making is an approach for assisting Individuals Experiencing Learning Difficulties to make choices. The Client is assisted to make important decisions either by a particular group of Significant Others or a Specific Other ( perhaps a family member or a Carer). The role of those supporting is NOT to make the decision on behalf of the Learner but to help him/her to:
- gather information;
- evaluate the options;
- consider the consequences of each choice.
Substitute decision-making involves an advocate acting on behalf of a Client in his or her 'best interest'. If the Client was believed to be incapable of understand the varying aspects of the choice or was so ill as to be temporarily incapacitated, a Significant Other (or Others) might be asked to make a decision on the Client's behalf.
Hobson's Choice refers to the 1915 play by Harold Brighouse and four subsequent films of the same. However, it's origins date back to the mid to late 16th century to Thomas Hobson, a livery stable owner, who was reputed to have given his customers 'no choice': they could either take a specific horse from a specific place or leave with nothing at all. Hobson's choice is therefore no choice at all (Here's some tea) perhaps made on a belief that this is what the Client wants (without any real evidence) but, more likely, at the whim of another or to meet the restraints the residence itself (We can only find tea, so everyone must have tea!).
At different times of the day, and faced with different types of decisions, a Client may encounter every type of choice on the continuum:
- at breakfast, s/he may make an independent choice of a contained set of drinks with family;
- when Carers arrive in the morning, s/he may make a supported choice on some aspect of a future event;
- during a hospital visit a spouse may decide on the best course of action regarding a particular medical issue;
- a trip out with the family in the evening may be to see a film decided by another member of the family with no reference to the Client.

57. Advocate an advocate. If Clients are unable to speak for themselves (or lack the cognitive capacity to communicate an understanding of the situation), an advocate (Davis, 2006) may speak on the Client’s behalf. Try to ensure that an advocate is present at least once a week to monitor practice and provide feedback on behalf of the Client. The Mental Capacity Act (2005) states that people can no longer make decisions on behalf of others without following a process. The process states that any act of substituted decision-making must be in the best interest of the individual. That is, if someone other than the Client makes a decision on his or her part, it must be in the Client’s best interest. Although, it fails to define ‘best interest’.
58. Night and Day. From my point of view, there is, no longer, a difference between the day and the night. I tell a lie, the Carers come during the day and I have meals during the day. Other than that, there is, for me, no difference. I am not saying that I am unable to tell the time of day: I have a clock, with an illuminated readout, by my bed that not only tells the time but the display shows morning or afternoon as well as the day, date and year. All in bright, white, large, capital letters as if it was shouting at me to ensure I am aware of every aspect of the time! No, I am aware of the time. What I mean is that there is very little discernible difference between me during the day and me during the night. I can be asleep in the day and awake throughout the night. I can be working or playing on my computer, watching Netflix, or Prime, or YouTube, or reading at any time of day. I can be working on this paper at three in the morning or three in the afternoon. Time has much less meaning since my stroke. My room changes very little from day to night. It is at a constant temperature of 21 degrees centigrade. The lighting is from a small table lamp 24/7, which I rarely turn off. The curtains are shut continuously (my room is directly on the Street and I value privacy) and therefore the light does not vary. Overall, the day and night, for me, are almost the same. That being the case, I may fall asleep at any time.Carers are unsure what to do if they arrive and I am asleep. What would I advise in this circumstance? Leave asleep or awaken? My advice is to ask a Significant Other, if one is available, a spouse or family member. If such a person is not available then wake the Client. Better still, allow the Client to decide! On a previous call, ask the Client (while awake) what s/he would want a Carer to do in that situation: leave asleep or wake the Client? The Client chooses. Client choice is a means of control. The Client is in control of the situation even when asleep!
Eating and Drinking

59. Food glorious food. If there is a requirement to assist a Client with eating and drinking (Corcoran 2005; Heaven, Bamford et al 2013) there are a number of techniques that may prove useful.
- Dysphagia (problems with swallowing) (Foley, Teasell et al 2008; Cohen, Roffe et al 2016) is likely to be an issue with some Clients. Do not pretend to know how to cope in such a situation. Always seek professional advice. Speech and Language Therapists (SLT) usually have expertise in this area.
- Thicken drinks using a thickening agent, usually in the form of a powder added with a provided scoop. Adding more scoops of this powder and mixing into the drink will make it thicker. The Client Centred Care Plan should detail the Client mealtime regime. Typically, from one to four scoops per drink, four turning the drink into a sort of gelatinous substance somewhere between a liquid and a solid. Adding thickener also changes the drink’s flavour somewhat; the more scoops, the less flavour. However, it is a price worth paying if it helps prevent aspiration by making the drink more manageable and assists swallowing.
- Since my stroke, I have found it very difficult for my mouth to deal with extremes of temperature. I cannot cope with hot drinks or drinks straight from the fridge; those, I have to let stand until they reach room temperature. I do not know if this is an issue (with all who are in a similar condition to mine) but it is worthwhile asking the Client about drink temperature. The same is true of foods also. I have to wait until hot meals cool before attempting to eat them. It can take me over an hour to eat a meal. I am in bed and cannot sit up properly and, thus, attempt my meals whilst almost lying down flat with my head and shoulders raised a little. Not an ideal position for this purpose but one that presently I am forced to accept. My meal is usually cold long before I finish eating.
- As with drinks, select food carefully to aid the Client during the process of eating. Avoid some food completely if the client has difficulties in their management. Really dry and crumbly or flaky foods such as crisps (potato chips) and many biscuits may be out of bounds for quite some time. The SLT will be able to advise. Recommendations for foods to avoid should be contained in the Client’s Care Plan.
- Ensure the food is at the perfect temperature for the Client; the Goldilocks temperature, not too hot neither too cold. Allow the Client to perform a tongue test on the first spoonful to check the temperature. Hold a spoonful of food just in front of the Client’s mouth and encourage the person to test its temperature with the tip of their tongue. “Is it OK?” If the Client indicates ‘no’, ask closed questions to establish what is wrong. A closed question is one that can be answered with a ‘yes’ or a ‘no’. Do not ask, “How is it?” that is an open question which requires more than a simple yes/no response. Rather ask, “Is it too hot?” and await a response. The response need not be in the form of a spoken word, it may be a simple movement. If too hot or too cold, take the appropriate action to remedy the situation as quickly as possible.
- Eating and drinking, while lying in bed, are problematic and potentially dangerous. The Client should be sitting as upright as possible to reduce the risk of aspiration.
- Establish a simple method for the Client to indicate that s/he is ready for the next spoonful. Remember, the goal is control, so put the person in control over the rate of food delivery. This equally applies to giving any form of medication.
- Ensure the spoon goes into the mouth. Make it as easy as possible for the Client to manage this process.
- To minimise the possibility of choking, do not overload the spoon. Rather too little than too much. After assisting with one or two meals, establish the correct amount per mouthful.
- Ensure the Client clears his / her mouth of all food before presenting the next portion for the Client to take.
- We all have foods that we do not like. The Client will not like some foods also. Keep a record of disliked items and add these to the Client’s Care Plan for future reference.
- Allow plenty of time for the Client to chew and swallow.
- A Client may have difficulty with chewing. Present the meal in easily managed pieces. The Client may also find it difficult to keep every bit of food in his / her mouth, not having sufficient lip control to avoid drooling. Have wipes ready for this purpose. Always ask if it is all right to wipe / clean the Client. Obtain permission before performing this action.
- The Client may have a dietitian or a speech and language therapist who has assessed and provided guidance on suitable foods, consistency, and foods to avoid. This information should be in the Client’s Care Plan. Ensure that it is studied.
- If a person shows any signs of choking or discomfort of any kind whilst eating or drinking, stop and seek further clarification from a superior or professional attached to the Client. Their contact details should be in the Client’s Care Plan. Aspiration can be dangerous and therefore proceeding, when the person is clearly having difficulties, is foolhardy. Aspiration occurs if something enters a person’s airway or lungs by accident. It may be food, liquid, or some other material. This can cause serious health problems, such as pneumonia. Aspiration can happen if the Client has trouble swallowing normally. Trouble swallowing is known technically as dysphagia.
- The Client should decide when s/he is replete and has finished eating. Do not encourage the person just to ‘have a few more mouthfuls’ to clear the plate. The Client is in control. Avoid mentioning any uneaten food unless asking if the person wants it saving for a later time.
- Use a menu plan where possible. It should provide for a variety of suitable and nutritious meals.
- Control implies choice. Allow for Client choice whenever possible.
- A Client may choose an unhealthy option for every meal. Chips with everything! Presenting the Client with a choice of healthy options at the start should help avoid this. The goal is control.
- A Client may require some form of clothes protection whilst eating. Do not refer to this item as a ‘bib’. Protect the Client’s dignity as well as clothes by using an age appropriate term (dining apron, clothes protector, surcoat, tabard) for this item at all times.
- There is a significant chance of aspiration when assisting a Client who requires a drink. Ensure that the Care Plan is read and understood. Is there therapist guidance? Body position, drink thickness (thickeners may need to be added), drink temperature, drink presentation, and drink container may all require special attention. If you do not know what you are doing. Stop! Seek advice. This action may require further training. Always seek professional guidance. A Speech and Language Therapist will be able to provide support to ensure mealtimes are safe, enjoyable and provide sufficient nutrition.
- It is important not to force a Client to eat or drink. This will only make the process more difficult. Try to make all mealtimes as enjoyable an experience as you can. Take your time; never rush a drink or a meal.
- Pretend not to mind the Client not eating or drinking, even if it is annoying or frustrating. Never show signs of anger or frustration. Remember, the Client is in control. Empathy and patience are virtues worth cultivating.
- If a person consistently refuses food or drink, ensure you notify someone who can act on the situation. Do not attempt to address the issue yourself; always seek professional advice.

60. Out of date. I heard from one of my Carers that, she had witnessed another Carer going through a Client’s refrigerator and throwing away any out of date items, even if the produce was only out of date by a day or so. She had done this without any permission from the Client. Even if a product is two years out of date, it is not your decision as to whether it should be discarded. The Client is in control. It is the Client who decides whether an item is to be kept or discarded. The Client’s alone, although as a responsible Carer, you should provide advice to the Client to help the Client reach a decision. If the Client decides to keep the product and asks for it to be prepared, you are within your rights to inform the Client politely that you cannot do anything that would put her / him in danger, even if the danger is small or uncertain. If the Client’s choice is D.U.B.I.O.U.S. (see earlier this page) you have the right to overrule it.
Consultation and Coordination (Post-Stroke Provision)
61. Pain management. While the stroke itself did not really cause me much pain (it was over in seconds), the aftermath, the days, weeks, and months post –stroke, were filled with frequent episodes of intense pain. Pain in my left arm and leg, pain when my leg began to spasm (which it did several times each day), pain from my catheter, pain from bypassing, pain from constipation, pain from continual pressure on my bottom as a result of my stationary position, pain from my mouth, the left side of which felt ‘alien’ following the stroke. One form of pain would set off another and that would cause my leg to spasm and my foot to tense painfully, in a cruel chain of increasingly painful events. It is essential, therefore, that there is good post-stroke pain management. (Bowsher 1995; Hansson 2004; Henon 2006; Widar, Ek, & Ahlström 2007; Kim 2014; Mulla, Wang et al 2015; Choi‐Kwon, Choi et al 2017). No doctor has ever been to see me to assess my needs and formulate a Post-Stroke Management Protocol (PSMP). Each time I have been in serious pain, it has been up to my wife to ring the doctor and book a ‘telephone consultation’. A few times, we have had to tell the doctor the name of the medication I needed prescribing. Ringing the doctor and booking a call back is not an example of good practice. I would wait for hours, still in pain, until the end of surgery for a doctor to call and, on each occasion, my wife had to explain my condition to the doctor. It is not a very helpful system for a person in my position. A lot of time and effort could have been saved by a PSMP initiated on my discharge from hospital. Ongoing pain affects the quality of life of the individual and can result in post-stroke depression (Kong, Woon, & Yang 2004; Jensen, Chodroff, & Dworkin 2007; Şahin-Onat, Ünsal-Delialioğlu et al 2016; Kwon 2017; Payton & Soundy 2020). Hospitals should have a continuing duty of care, to the acute stroke Patients whom they discharge, at least, in the first six months.
62. Quality control. Is there adequate monitoring of care services? (de Waal 2008) Each day, I have three care calls involving two Carers per call. The same two people generally do not staff the calls; it can be different combinations every time. Sometimes a complete stranger arrives! The quality of service provided by individual Carers varies enormously. One Carer rarely speaks and never says ‘hello’ whilst others are the complete opposite. Standards vary a lot from Carer to Carer and nobody seems to be monitoring my provision. Consistency is important. Quality is important. Care provision should aim to deliver both. Schools are inspected regularly, the quality of provision being important. There is even regular, ‘in house’ quality checks to ensure standards are maintained. I suspect this happens as standard in other professions also. The Care Quality Commission (CQC) appears to be the regulatory body ensuring standards in home care provision. I just looked at their website to see what they say about my Care Company. I found it and it states that, 'We have not inspected this service yet.' I hope my service is inspected soon and the customer gets to give an opinion.
The Client, who has to pay for the service, cannot simply stop and move to another care provider company because it is quite difficult to get any provision. I have experienced two different care companies and virtually all the same issues occurred with both. I have no reason to believe that similar issues would not occur with any other company that I chose to employ. I have real concerns for aged non-verbal Clients under a provision financed by other than the Client (local council?) whom no one monitors for quality and the standard of service in place. Not every call is bad, far from it – some Carers provide excellent care and most are adequate. However, even the Carers that I would rate as outstanding, make a few of the ‘mistakes’ reported in this paper. I suspect that their training was not thorough and, after initial training, there were no subsequent training sessions. While, learning on-the-job is one form of training provision, if it is not supported with regular in-house training to review what has been learned, bad habits can easily become standard working practice. Quality of life is dependent on quality of provision. What is your employer doing about it? The CQC appears to monitor across five areas: safe, effective, caring, responsive, and well led. Each area is given one of five ratings after the inspection: outstanding, good, requires improvement, inadequate, and no rating given / rating under appeal / rating suspended. An overall rating is finally provided based on an analysis of the former results. As far as I can tell, the majority of local care providers have a ‘good’ rating (148) following inspection, with 29 that ‘require improvement’ and, only four (out of 279 in total) receiving the ‘inadequate’ result (at the time of writing). I am surprised that so many were rated as ‘good’ when the two with which I have experience, I would rate as ‘requiring improvement’. I wonder what experience the inspectors have and if any are IRONs or POD in the role? People with experience of receiving care. I have been asking my Carers if their practice had ever been inspected. One excellent Carer had been working for my Care Company for 22 years and said that she had never been inspected or even had her practice observed by the Company (although other Carers reported that they have had a senior Company member doing inspections). She reported that, as far as she was aware, the CQC only ever go into the office and look at the books. Each of my Care team I asked said that their practice had not been observed (by the CQC). If what they told me is factual, I think that standards in the quality of care provision have little chance of improving. They did report that they have had training on various topics; moving and handling, medication, etc. However, someone like me, an actual recipient of care, had never provided the training. I find that it all ‘requires Improvement’! It is poor if quality of care is measured only as a standard of recording in documents (that have been generated by the Companies and their care teams themselves). They are hardly likely to put in print anything negative about their practice, with even problematic events receiving a bias and positive gloss. Obviously, the focus should be on the care provided itself, anything less falls short of the mark. It is hardly surprising that there are so many ‘good’ ratings if the actual practice in the homes of Clients is not observed. At the very least, Clients should be asked if they would be willing to provide the Care Company a report on their view of the quality of their provision four times annually. The Company should keep Client reports such that they may be scrutinised by the inspectorate. IRONs should have a voice. Otherwise, they become ‘Clients in the IRON mask’. Personally, I would be more than willing to be interviewed by an inspector or even have inspectors view the quality of my care provision. So many people have seen me naked since my stroke, what are a few more going to matter to me? When my Care Company finally are inspected, I would not be surprised if they get a ‘good’ grading under the current system. If I were to grade them, presently, I would say that the Care Company ‘requires improvement’. Indeed, the whole post-stroke provision in my area requires improving! My hospital proudly displays a plaque in the entrance which states that it has been awarded an Outstanding rating by the CQC. Outstanding, really?
The Client, who has to pay for the service, cannot simply stop and move to another care provider company because it is quite difficult to get any provision. I have experienced two different care companies and virtually all the same issues occurred with both. I have no reason to believe that similar issues would not occur with any other company that I chose to employ. I have real concerns for aged non-verbal Clients under a provision financed by other than the Client (local council?) whom no one monitors for quality and the standard of service in place. Not every call is bad, far from it – some Carers provide excellent care and most are adequate. However, even the Carers that I would rate as outstanding, make a few of the ‘mistakes’ reported in this paper. I suspect that their training was not thorough and, after initial training, there were no subsequent training sessions. While, learning on-the-job is one form of training provision, if it is not supported with regular in-house training to review what has been learned, bad habits can easily become standard working practice. Quality of life is dependent on quality of provision. What is your employer doing about it? The CQC appears to monitor across five areas: safe, effective, caring, responsive, and well led. Each area is given one of five ratings after the inspection: outstanding, good, requires improvement, inadequate, and no rating given / rating under appeal / rating suspended. An overall rating is finally provided based on an analysis of the former results. As far as I can tell, the majority of local care providers have a ‘good’ rating (148) following inspection, with 29 that ‘require improvement’ and, only four (out of 279 in total) receiving the ‘inadequate’ result (at the time of writing). I am surprised that so many were rated as ‘good’ when the two with which I have experience, I would rate as ‘requiring improvement’. I wonder what experience the inspectors have and if any are IRONs or POD in the role? People with experience of receiving care. I have been asking my Carers if their practice had ever been inspected. One excellent Carer had been working for my Care Company for 22 years and said that she had never been inspected or even had her practice observed by the Company (although other Carers reported that they have had a senior Company member doing inspections). She reported that, as far as she was aware, the CQC only ever go into the office and look at the books. Each of my Care team I asked said that their practice had not been observed (by the CQC). If what they told me is factual, I think that standards in the quality of care provision have little chance of improving. They did report that they have had training on various topics; moving and handling, medication, etc. However, someone like me, an actual recipient of care, had never provided the training. I find that it all ‘requires Improvement’! It is poor if quality of care is measured only as a standard of recording in documents (that have been generated by the Companies and their care teams themselves). They are hardly likely to put in print anything negative about their practice, with even problematic events receiving a bias and positive gloss. Obviously, the focus should be on the care provided itself, anything less falls short of the mark. It is hardly surprising that there are so many ‘good’ ratings if the actual practice in the homes of Clients is not observed. At the very least, Clients should be asked if they would be willing to provide the Care Company a report on their view of the quality of their provision four times annually. The Company should keep Client reports such that they may be scrutinised by the inspectorate. IRONs should have a voice. Otherwise, they become ‘Clients in the IRON mask’. Personally, I would be more than willing to be interviewed by an inspector or even have inspectors view the quality of my care provision. So many people have seen me naked since my stroke, what are a few more going to matter to me? When my Care Company finally are inspected, I would not be surprised if they get a ‘good’ grading under the current system. If I were to grade them, presently, I would say that the Care Company ‘requires improvement’. Indeed, the whole post-stroke provision in my area requires improving! My hospital proudly displays a plaque in the entrance which states that it has been awarded an Outstanding rating by the CQC. Outstanding, really?

63. Time Critical (Kiley 2014). I am paying for three care calls a day; one early morning, one midday, and one in the afternoon at three thirty. The cost of care is expensive but the service I receive mostly falls far short of excellent (some is very good). The time of the afternoon call can vary by as much as an hour. I have had Carers arrive at before three o’clock and, on different days, as late as four. I realise that there may be staffing issues, staff can become ill and then not turn up for work, or a delay can occur for a myriad of understandable reasons. However, there is no excuse for not calling to let me know. Today, the Carers arrived thirty minutes later than normal. When I queried the late time, the Carers replied that the Care Company schedule informed them to arrive at that time. The Care Company had made no effort to contact me and let me know of the time change. Each month I receive an invoice for the service and, somewhere in the listing, it always reads, “Time critical call” but the times listed are not the same. Thus, a ‘time critical’ call can be at a specific time one day but at a quite different time on others. The Company is lacking in professionalism, if there was an inspectorate worthy of the name, they would almost certainly be placed in ‘special measures’. The trouble is, there are so many people in need of care services and only a few companies serving the market. It is not easy to find and set up a care package. When my wife was trying to sort out my provision, she tried several companies. Some were fully booked and could only guarantee provision of care if an existing Client was to ‘cease use of their service’. Some were charging over a thousand pounds a week and we just could not afford that level of payment; our retirement savings would not last much more than a year or two before we would be penniless. Some companies charged double for Sundays and for all holiday periods and (to add insult to injury), if the customer did not need the service for a few days, payment was still required! As a result of financial constraints, and other issues, our choice of Care Company was restricted. We had little time to ‘shop around’ because the hospital kept calling demanding to know when we were going to start with our own care plan such that they could terminate their provisional post-hospital package which they were financing. Our world had changed drastically yet, at a time of great stress, we were coerced into making a quick decision with little help or counselling. A post-stroke counselling service would have been a great help in the early days when we had very little idea what assistance was available. If such a body exists, we were not aware of it and my wife struggled through the early days mostly on her own. I was of little help as I was fighting pain for much of the time. Just a person who had some level of expertise who came every day for a few days to provide advice and support would have helped enormously. Someone who might guide us in the selection of a Care Company and recommend one with a good standard of service. There is little incentive for Care Companies to improve standards. My wife has complained, in writing, a number of times and the Care Company suggested a review but weeks have passed and nothing has happened. Care Companies should face penalties for not meeting basic standards of practice. Mine is but a lone voice shouting (if I could shout) in darkness but, if enough people read this and act, perhaps something will change. I cannot be the only person receiving care who has issues with the quality of provision. I sometimes have a male Carer. While the female Carer arrives at one time, the male arrives up to ten minutes later. My care requires two Carers working together. When only one is present, she has clocked in on arrival. My half hour slot then begins. If the second Carer arrives late, both Carers leave together after the half hour. Thus, I have lost care time for which I still am charged. The late Carer shows no concern over the issue. Indeed, one Carer simply walked out while I was explaining the problem knowing that I could do nothing about it.
64. To bed, to bed, sleepy head. When I left hospital, I was provided with a hospital style bed complete with mattress. I was (and still am) very grateful for this provision. At the time, I was unaware of my continuing needs. However, as days turned into weeks and weeks into months, I began to comprehend just how the bed provided was failing to meet my needs. Soon, after hospital, I realised that, while my bed has a function to lower the bottom (such that my feet are lower than my head), it did not have a function to lower the top (my head in respect to my feet). I was slipping down the bed as I used its various features throughout the day and required others to reposition me several times a day. This involved rolling me to position a slip-sheet underneath my body (which is used to aid movement of a body by reducing friction). The process required two Carers working together. When the Carers were not present to assist with this matter (which was the majority of the day), it fell to my poor wife to try to drag me up the bed on her own. I am not overweight but, even so, it was a strenuous task for my wife on her own. If she hurt her back, who would be around to help? I learned that the head lower than the feet position is known as the Trendelenburg function. The position is named after the German surgeon Friedrich Trendelenburg (1844–1924). A reverse Trendelenburg position has the feet lower than the head. For an IRON, a Trendelenburg function is a necessary requirement for a suitable bed. The requirement is as much for the person’s spouse as it is for the Client. It significantly eases the aforementioned repositioning task and reduces likelihood of Carer injury. My condition means that I am incapable of rolling onto either side of my body unaided. The Care Company insists this procedure requires two Carers to prevent injury to those assisting. Carers are able to wash specific areas of my anatomy whilst I am on my side and are only able to deal with certain other bodily functions while I am in this position. When two Carers are not in attendance, it (once again) falls to my wife to attempt to roll me and hold me on my side (I have a tendency to topple back onto my back, when on my right, if not held in place by some means). This requires one hand to hold me and the other to try to perform whatever task is necessary. It is very difficult for my wife acting on her own. Again, this task raises the chance of injury. A bed can have a function to tilt a Patient laterally to either side to ease this process considerably in the instance where only a single Carer is available. The luxury of having two Carers in attendance, in my household, happens for one hour fifteen minutes each day. For the remaining twenty-two hours and forty-five minutes, my wife is my sole Carer. When I began to develop pressure sores, I involved the local nursing service. They ensured that I had a change of mattress to one designed specifically to better cope with the issue. Surely, it was possible to foresee the probability of development of pressure sores, for a person with my level of disability, while I was in hospital and the correct mattress for use by an IRON provided initially. The lack of functional capability of my bed became more of an issue over time. I was not able to sit upright whilst in bed to eat or drink. To get me out of bed and into a chair of any description continues to involve a number of actions that take time and effort. Initially, I could not sit on any chair for longer than a few minutes without becoming increasingly uncomfortable and with growing pain. This was realised while I was in hospital because therapists worked to improve my tolerance to being sat in a chair. There are beds that are able to adopt a chair like position safely at the touch of a button. Whilst my current bed is able to approximate a chair function, it is not at the touch of a button and I find it uncomfortable. As I became increasingly frustrated with the lack of functionality of my bed, I started searching on-line for something more suited to my requirements. I discovered a whole host of amazing beds with much more functionality. I began emailing companies to enquire about the purchase of this item. I realised that such a bed would likely cost me thousands of pounds but, as I would likely spend a considerable amount of time in bed in the future, and comfort and health are extremely important to me, the money was not the first thing on my mind. My wife and I have saved all our lives and planned for our retirement (although we had not considered that I would be spending it as a POD. Although the money would considerably eat into our savings, we both agreed it was worth the expense. However, I received a phone call from one company to inform me that it was against their policy to sell a bed into a residential household. They went on to explain that if I were to employ a full-time nurse there was no problem. I found the refusal to allow me to purchase a bed that I wanted very troubling. Informed that it could, however, be supplied if I was to employ a nurse full-time really made me angry. It implied that my wife and I did not have the intelligence or the ability to master the bed control and my care safely. I have a Master's degree and my wife is also educated to degree level. Furthermore, I have had a hospital-style bed for eleven months and not a single hospital nurse has set foot anywhere near my home. My wife and I have to manage my care without any hospital help whatsoever (except for a thirty-minute visit from a brilliant physiotherapist once a fortnight and some basic follow-up information in the first couple of weeks). We have not had one incident with my bed in eleven months and my care is totally in our hands. I was further informed that the Trendelenburg function is a safety issue not permissible in a residential setting. However, other companies were willing to provide a bed with this function, so there was some issue with that claim. I emailed the company concerned following the call to complain and raise issues of discrimination against individuals of disability residing at home. I pointed out that they had just lost a customer and several thousands of pounds for the purchase. I noted that, although the company may view itself as applying the highest standard to the sale of its merchandise, it was discriminating against POD (such as myself. I am an IRON POD!) who would be perfectly good customers. I also wrote to my MP, several media outlets and a few other people to highlight the issue because I genuinely believed it to be discrimination and, if it is law, then the law requires changing. My grievance is with any form of discrimination against POD, no matter the rationale. To cite health and safety as a reason, when clearly my health and safety issues are being adequately managed already without any nursing assistance post-stroke via a local provision (there isn't any; it feels like we have just been abandoned), is somewhat ironic.
65. Air on a bed spring. Above, I noted that I have a Royal System alternating pressure relieving mattress system. It is an air mattress specifically designed to reduce the possible development of pressure sores. It comprises a number of sausage shaped segments that run from side to side. A pump situated at the bottom of the bed alternately inflates, first, the odd segments and then, the even. Thus, the mattress is continually changing the surface contour and its pressure. A ingenious idea except I slept on it for two days and nights (or, to be precise, didn’t sleep) and found it to be both uncomfortable and to hurt my bottom. I had to use two memory foam mattress toppers and a soft fleece under blanket on top of the air mattress just to make it comfortable. I also used two memory foam cushions;one under each buttock, to relieve pressure off my bottom. These cushions work for an hour or two but then, they become so compressed under my weight, it feels as if I am sitting on a solid floor. Usually, by the time I am beginning to feel uncomfortable with my cushions, the next pair of Carers arrive and can sort me out. I think a pressure relieving mattress is overkill for my particular problem. It attempts to relieve pressure over its entire surface, top to bottom. I only have an issue with my behind and the remainder of the mattress is just serving to make me uncomfortable. What I believe I need are two inflatable cushions joined together down one side. The inflation of the cushions would be controlled via a simple four button Client control pendant. The Client is able to both adjust the inflation (up or down) of the right cushion and to adjust the inflation (up or down) of the left cushion. The Client would be in control. If the Client’s bottom began to feel uncomfortable, the Client could then make the necessary adjustments to rectify the situation. The Client would not be able to over inflate either cushion because the system would have a maximum inflation setting. My present air pump hangs off the bottom of my bed. It is in operation constantly 24/7. It is noisy and the noise affects my sleep. Furthermore, it vibrates the board at the foot of my bed. If my bad left foot comes into contact with the vibrating board, it triggers a spasm which is painful. As I have no control over my left leg, I cannot move it off the footboard and the vibrations and the spasms continue. In this situation, I raise the knee break on the bed which takes my foot off the board. I have the knee break raised until the Carers arrive and can pull me further up the bed and my feet away from touching the footboard. The air mattress system is expensive. It is also, in my opinion, badly designed. The pump is noisy and vibrates and the mattress itself is uncomfortable. Pressure sores are quite literally a pain in the bum but the system, used to alleviate the problem, comes with additional issues.
66. Summation. It is my opinion, based on nearly a year's post-stroke experience, that post-stroke provision (in my area at least and, I suspect, in others as well) requires significant Improvement. I would recommend the following:
- Hospitals initiate a Post-Stroke Management System with staff to oversee the quality of provision both in hospital and at home following discharge for a period of not less than six months, with an option to extend should it be necessary.
- Each Patient on the scheme be allocated a Case Manager to be the point of contact for the Patient and family. The Case Manager would have sufficient knowledge to be able to advise on services that provide support, on care providers, on equipment that might be of assistance, on assuring the correct level of therapy support is provided, on financial concerns (grants and allowances), on pathways to improved outcomes, and on all things stroke related. The Case Manager would also be responsible for the care of other family members especially those providing care. The initial period following the discharge from hospital can be overwhelming for families and they require support from an able person.
- Necessary equipment for home care be under continuing review and upgraded as necessary. Unused or unwanted equipment removed.
- Each Patient on the scheme be allocated a doctor to initiate and oversee a Pain Management System in liaison with the Patient's own doctor. The doctor to be on call should the Patient ever be experiencing prolonged periods of pain of an hour or more. The doctor to take responsibility for the ongoing prescription of necessary medication and provisions (catheters, incontinence pads, wipes, plasters, etc.)
- Post-Stroke Pressure Sore Management seeking 'prevention of' rather than 'treatment for'. All IRON POD are in the at-risk category of Patients and will be eligible for this service.
- At-home post-stroke therapy (Speech, Occupational, Physio, and mental health Counselling) is provided on a weekly basis, as necessary, for a period not less than one year.
- Regular inspection of quality of provision.
- Each Patient has a regular review where all involved parties meet to discuss progress.
- The Patient is able to contribute to the review either in person or by proxy, or with a written statement.
- Each Patient / Client be given the opportunity to report on care provision quarterly direct to the CQC via an online form. The data kept secure for the Care Company review.
- Each Patient be given the opportunity to report on in-hospital nursing care provision to the P.E.T. at any time. The report to be treated seriously with reprimands for staff where necessary.
- All provision, grants, allowances to be on an as needed basis and not means tested. People who have been sensible and planned for their retirement should not be penalised for having savings. If they have been paying National Insurance contributions on a regular basis for ten years or more, they should automatically qualify for the scheme.
67. Update
A year passed since my hospital stay following my stroke. I am still bed bound and suffering from periods of pain. I became ill and had to go back into hospital once again on Sunday 24th October 2021 after having trouble with my catheter and my bladder, as well as a chest infection that caused me to have a rather rattly chest and to cough a lot. My wife called the nursing services and also dialled 111 for medical support in the UK. Nursing services sent a nurse who changed my catheter. However, that made little difference to my condition and the pain I was experiencing. 111 arranged for a doctor to visit. The doctor arrived soon after the nurse had left. He examined me thoroughly and concluded that I had both a bladder and a chest infection. He also thought that I was in the early stages of sepsis. He called for an ambulance to take me to hospital. It arrived within an hour of his call and I was taken the few miles to King’s Mill Hospital, Sutton in Ashfield and rushed into the emergency department where I was assessed and admitted as a patient for (initially) an overnight stay. I spent just a few hours on the emergency ward where I was given a lot of tests including an x-ray of my chest, blood analysis, urine analysis and poked and prodded quite a bit. I was given a Covid test (which, I am pleased to say, was negative). A cannula was inserted into my right arm which, I have to say, hurt more than I thought it would! Following all of that, I was transferred onto a general ward in a small single room. It was now around midnight and more nurses appeared to repeat the tests and checks done earlier. I was very tired by this point in time but, after an hour or so, I was transferred, yet again, to another small room on the same ward. It was after 1 o’clock by this time and yet another nurse appeared to attach a saline drip and an antibiotic drip into the two connections on my cannula. A further nurse came to give me more medication and yet more nurses made me comfortable for the rest of the night. I don’t remember much after that, I must have fallen asleep. I was awakened by two doctors who informed me that my tests had shown I had both a bladder and a chest infection which could be treated with a course of antibiotics (directly into my cannula)and additional problems but nothing about which I should worry. They explained that I would have further tests done that day and, all being well, I could go home on Tuesday.
Lots of things happened on the Monday (both good and bad) some of which I have already detailed. Tuesday morning arrived and I was seen by another doctor (that brought the tally of different doctors I had seen since Sunday evening to five.) who told me pretty much the same thing, I would have more tests done and, if all was well, I could go home later that day. I hate hospitals having had horrible experiences in them on my previous two visits (detailed on this page. One for several weeks following my stroke and another for several days shortly afterwards when I had a chest infection caused by my poor swallowing ability and liquids entering my lungs.). I have said that hospitals are, for IRON PODs (Individuals Reliant on Others for Needs • Person Of Disability), not places to be when you are ill and a stay there should be as short as possible. My experiences in the short time I was in hospital this time were mostly not positive. Before going into hospital, I was receiving two visits a week from nursing services to flush my catheter and continue the care of the pressure sores on my bottom. I was in hospital approximately 48 hours. On returning home, the twice weekly nursing service stopped. No nurse came to call. After a week my wife rang to ask why no nurse had been to call. She was informed that the service was stopped when I went into hospital and the hospital had not notified them of the necessity to restore the provision following my discharge. No communication and so, no service! Yet a further example of the poor post-stroke provision in my area.
A year passed since my hospital stay following my stroke. I am still bed bound and suffering from periods of pain. I became ill and had to go back into hospital once again on Sunday 24th October 2021 after having trouble with my catheter and my bladder, as well as a chest infection that caused me to have a rather rattly chest and to cough a lot. My wife called the nursing services and also dialled 111 for medical support in the UK. Nursing services sent a nurse who changed my catheter. However, that made little difference to my condition and the pain I was experiencing. 111 arranged for a doctor to visit. The doctor arrived soon after the nurse had left. He examined me thoroughly and concluded that I had both a bladder and a chest infection. He also thought that I was in the early stages of sepsis. He called for an ambulance to take me to hospital. It arrived within an hour of his call and I was taken the few miles to King’s Mill Hospital, Sutton in Ashfield and rushed into the emergency department where I was assessed and admitted as a patient for (initially) an overnight stay. I spent just a few hours on the emergency ward where I was given a lot of tests including an x-ray of my chest, blood analysis, urine analysis and poked and prodded quite a bit. I was given a Covid test (which, I am pleased to say, was negative). A cannula was inserted into my right arm which, I have to say, hurt more than I thought it would! Following all of that, I was transferred onto a general ward in a small single room. It was now around midnight and more nurses appeared to repeat the tests and checks done earlier. I was very tired by this point in time but, after an hour or so, I was transferred, yet again, to another small room on the same ward. It was after 1 o’clock by this time and yet another nurse appeared to attach a saline drip and an antibiotic drip into the two connections on my cannula. A further nurse came to give me more medication and yet more nurses made me comfortable for the rest of the night. I don’t remember much after that, I must have fallen asleep. I was awakened by two doctors who informed me that my tests had shown I had both a bladder and a chest infection which could be treated with a course of antibiotics (directly into my cannula)and additional problems but nothing about which I should worry. They explained that I would have further tests done that day and, all being well, I could go home on Tuesday.
Lots of things happened on the Monday (both good and bad) some of which I have already detailed. Tuesday morning arrived and I was seen by another doctor (that brought the tally of different doctors I had seen since Sunday evening to five.) who told me pretty much the same thing, I would have more tests done and, if all was well, I could go home later that day. I hate hospitals having had horrible experiences in them on my previous two visits (detailed on this page. One for several weeks following my stroke and another for several days shortly afterwards when I had a chest infection caused by my poor swallowing ability and liquids entering my lungs.). I have said that hospitals are, for IRON PODs (Individuals Reliant on Others for Needs • Person Of Disability), not places to be when you are ill and a stay there should be as short as possible. My experiences in the short time I was in hospital this time were mostly not positive. Before going into hospital, I was receiving two visits a week from nursing services to flush my catheter and continue the care of the pressure sores on my bottom. I was in hospital approximately 48 hours. On returning home, the twice weekly nursing service stopped. No nurse came to call. After a week my wife rang to ask why no nurse had been to call. She was informed that the service was stopped when I went into hospital and the hospital had not notified them of the necessity to restore the provision following my discharge. No communication and so, no service! Yet a further example of the poor post-stroke provision in my area.

68. Update
It is now July 2022. Almost two years post stroke and, the good news is that things are getting better. I'm not in so much pain, although I am still having problems with my bowels. I am trying to get into a routine. Every day I am going out in my new electric wheelchair just to practice maneuvering it accurately. I continue to spend the majority of my time in bed working on my computer as I am doing now. Things move very slowly but, there is some light at the end of the tunnel. I'm willing to help anyone unfortunate enough to find him/herself in the same situation following a stroke or some other illness. Use the form at the bottom of this page to make contact.
It is now July 2022. Almost two years post stroke and, the good news is that things are getting better. I'm not in so much pain, although I am still having problems with my bowels. I am trying to get into a routine. Every day I am going out in my new electric wheelchair just to practice maneuvering it accurately. I continue to spend the majority of my time in bed working on my computer as I am doing now. Things move very slowly but, there is some light at the end of the tunnel. I'm willing to help anyone unfortunate enough to find him/herself in the same situation following a stroke or some other illness. Use the form at the bottom of this page to make contact.
Bibliography and References
Adigun, O.O., Mikhail, A.G., Krawiec, C., & Hatcher., J.D. (2020) Abuse and Neglect. StatPearls Publishing
Akyuz, G., & Kuru, P. (2016) Systematic review of central post stroke pain: what is happening in the central nervous system? American Journal of Physical Medicine & Rehabilitation, Volume 95(8), pp. 618 - 627.
Alcusky, M., Ulbricht, C.M., & Lapane, K.L. (2018) Post-acute care setting, facility characteristics, and post-stroke outcomes: a systematic review. Archives of Physical Medicine and Rehabilitation, Volume 99(6), pp.1124 - 1140.
Alderman, N. (2013) Managing challenging behaviour. In Neurobehavioural Disability and Social Handicap Following Traumatic Brain Injury. pp. 191 - 224. Psychology Press.
Allen, K., Hazelett, S., Jarjoura, D., Wright, K., Clough, L., & Weinhardt, J. (2004) Improving stroke outcomes: implementation of a post-discharge care management model. The Journal of Clinical Outcomes Management. Volume 11(11), pp. 707 - 717.
Allman, R.M. (1997) Pressure ulcer prevalence, incidence, risk factors, and impact. Clinics in Geriatric Medicine. Volume 13(3): pp. 421 – 436
Ancheta, J., Husband, M., Law, D., & Reding, M. (2000) Initial functional independence measure score and interval post stroke help assess outcome, length of hospitalization, and quality of care. Neurorehabilitation and Neural Repair, Volume 14(2), pp.127 - 134.
Andrewes, H.E., Walker, V., & O’Neill, B. (2014) Exploring the use of positive psychology interventions in brain injury survivors with challenging behaviour. Brain Injury, Volume 28(7), pp. 965 - 971.
Aziz, A.F.A., Nordin, N.A.M., Ali, M.F., Abd Aziz, N.A., Sulong, S. & Aljunid, S.M. (2017). The integrated care pathway for post stroke Patients (iCaPPS): a shared care approach between stakeholders in areas with limited access to specialist stroke care services. BMC Health Services Research, Volume 17(1), pp.1 - 11.
Aziz, A.F.A., Nordin, N.A.M., Abd Aziz, N., Abdullah, S., Sulong, S., & Aljunid, S.M. (2014) Care for post-stroke Patients at Malaysian public health centres: self-reported practices of family medicine specialists. BMC Family Practice, Volume 15(1), pp.1 - 11.
Bainbridge, L. (2019) .A Complete Guide on How to Use a Hoist Correctly https://www.beaucare.com/blog/a-complete-guide-on-how-to-use-a-hoist-for-correctly/
Bakas, T., Austin, J.K., Jessup, S.L., Williams, L.S., & Oberst, M.T. (2004) Time and difficulty of tasks provided by family caregivers of stroke survivors. Journal of Neuroscience Nursing, Volume 36(2), pp. 95 - 106.
Barlow J., Wright C., Sheasby J., Turner A., & Hainsworth, J. (2002) ‘Self-management approaches for people with chronic conditions: a review’, Patient Education and Counseling. Volume 48: pp. 177 - 187
Barton, A., & Barton, M. (1981) The Management and Prevention of Pressure Sores. Faber and Faber, London
Bastawrous, M., Gignac, M.A., Kapral, M.K. & Cameron, J.I. (2015) Adult daughters providing post-stroke care to a parent: a qualitative study of the impact that role overload has on lifestyle, participation and family relationships. Clinical Rehabilitation, Volume 29(6), pp.592 - 600.
Bastemeijer, C.M., Boosman, H., van Ewijk, H., Verweij, L.M., Voogt, L., & Hazelzet, J.A. (2019) Patient experiences: a systematic review of quality improvement interventions in a hospital setting. Patient Related Outcome Measures, Volume 10, pp.157 - 169.
Beamer, S. & Brookes, M. (2001) Making Decisions – best practice and new ideas for supporting people with high support needs to make decisions. Values Into Action. London
Berg, A., Palomaki, H., Lehtihalmes, M., Lönnqvist, J., & Kaste, M. (2003) Post-stroke depression: an 18-month follow-up. Stroke, Volume 34(1), pp.138 - 143.
Berger, S., Saut, A.M., & Berssaneti, F.T. (2020) Using Patient feedback to drive quality improvement in hospitals: a qualitative study. BMJ Open, Volume 10(10), p.e037641.
Bernstein, S. (2017) Don’t tell an upset person “calm down.” Do this instead. Web page article at: https://drsusanbernstein.com/dont-tell-an-upset-person-calm-down-%E2%80%8B-do-this-instead/
Birbeck Nevins, J. (1895) The sign language of the deaf and dumb. Proceedings of the Literary and Philosophical Society of Liverpool
Boden-Albala, B.M.P.H.D., Litwak, E., Elkind, M.S.V., Rundek, T.M.D.P., & Sacco, R.L. (2005) Social isolation and outcomes post-stroke. Neurology, Volume 64(11), pp.1888 - 1892.
Boivie, J. (2006) Central post-stroke pain. Handbook of Clinical Neurology, Volume 81, pp. 715 - 730.
Boosman, H., Schepers, V.P.M., Post, M.W.M., & Visser-Meily, J.M.A. (2011) Social activity contributes independently to life satisfaction three years post stroke. Clinical Rehabilitation, Volume 25(5), pp. 460 - 467.
Bowsher, D. (1995). The management of central post-stroke pain. Postgraduate Medical Journal, Volume 71(840), pp. 598 - 604.
Broomfield, N.M., Quinn, T.J., Abdul-Rahim, A.H., Walters, M.R., & N Evans, J.J. (2014) Depression and anxiety symptoms post-stroke/TIA: prevalence and associations in cross-sectional data from a regional stroke registry. BMC Neurology, Volume 14(1), pp. 1 - 9.
Brown, I., & Brown, R.I. (2003). Quality of Life and Disability.. Jessica Kingsley
Brown, I., & Brown, R.I. (2009). Choice as an aspect of quality of life for people with intellectual disabilities. Journal of Policy and Practice in Intellectual Disabilities, volume 6 (1), pp.11 - 18.
Bryen D.N. (1993) Augmentative Communication Mastery: One approach and some preliminary outcomes. The First Annual Pittsburgh
Employment Conference for Augmented Communicators Proceedings. August 20-22: Shout Press: Pittsburgh
Burns, S., & Day, T. (2012) A return to the basics: interventional Patient hygiene (a call for papers). Intensive and Critical Care Nursing; Volume 28(4), pp. 193 - 196.
Bustamante, A., Garcia-Berrocoso, T., Rodriguez, N., Llombart, V., Ribo, M., Molina, C. & Montaner, J. (2016) Ischemic stroke outcome: a review of the influence of post-stroke complications within the different scenarios of stroke care. European Journal of Internal Medicine, Volume 29, pp.9 - 21.
Cairns, D., Williams, V., Victor, C., Richards, S., Le May, A., Martin, W., & Oliver, D. (2013) The meaning and importance of dignified care: findings from a survey of health and social care professionals. BMC Geriatrics, Volume 13(1), pp. 1 - 6.
Cameron, J.I., Cheung, A.M., Streiner, D.L., Coyte, P.C., & Stewart, D.E. (2011) Stroke survivor depressive symptoms are associated with family caregiver depression during the first 2 years post-stroke. Stroke, Volume 42(2), pp.302 - 306.
Cameron, J.I., Stewart, D.E., Streiner, D.L., Coyte, P.C., & Cheung, A.M. (2014) What makes family caregivers happy during the first 2 years post stroke? Stroke, Volume 45(4), pp.1084 - 1089.
Campbell, G.B., & Matthews, J.T. (2010) An integrative review of factors associated with falls during post‐stroke rehabilitation. Journal of Nursing Scholarship, Volume 42(4), pp.395 - 404.
Caro, C.C., Mendes, P.V.B., Costa, J.D., Nock, L.J., & Cruz, D.M.C.D. (2017) Independence and cognition post-stroke and its relationship to burden and quality of life of family caregivers. Topics in Stroke Rehabilitation, Volume 24(3), pp. 194 - 199.
Cassidy, E.M., O'Connor, R., & O'Keane, V. (2004) Prevalence of post-stroke depression in an Irish sample and its relationship with disability and outcome following inPatient rehabilitation. Disability and Rehabilitation, Volume 26(2), pp. 71 - 77.
Chan, H. (1997) Bladder management in acute care of stroke patients: a quality improvement project. Journal of Neuroscience Nursing, Volume 29(3), pp. 187 - 191.
Choi‐Kwon, S., Choi, S.H., Suh, M., Choi, S., Cho, K.H., Nah, H.W., Song, H., & Kim, J.S. (2017) Musculoskeletal and central pain at 1 year post‐stroke: associated factors and impact on quality of life. Acta Neurologica Scandinavica, Volume 135(4), pp. 419 - 425.
Clarke, D.J., & Forster, A. (2015) Improving post-stroke recovery: the role of the multidisciplinary health care team. Journal of Multidisciplinary Healthcare, Volume 8, p. 433.
Clark, M., Defloor, T., & Bours, G. (2004) A pilot study of the prevalence of pressure ulcers in European hospitals. In: Clark, M., ed. Pressure Ulcers: Recent Advances in Tissue Viability. Quay Books, Salisbury: pp. 8 – 22
Clark, M., Schols, J., Benati, G., Jackson, P., & Engfer, M. (2004) Pressure ulcers and nutrition: a new European guideline. Journal of Wound Care. Volume 13(7): pp. 267 – 272
Cohen, D.L., Roffe, C., Beavan, J., Blackett, B., Fairfield, C.A., Hamdy, S., Havard, D., McFarlane, M., McLauglin, C., Randall, M., & Robson, K. (2016) Post-stroke dysphagia: a review and design considerations for future trials. International Journal of Stroke, Volume 11(4), pp. 399 - 411.
Collins, A. (2014). Measuring what really matters: towards a coherent measurement system to support person-centred care. London: The Health Foundation. Available at: www.health.org.uk/publications/ measuring-what-really-matters/
Collins, F. (2000) Selecting the most appropriate armchair for Patients. Journal of Wound Care. Volume 9(2): pp.73 – 76
Comerford, C. (2015). Why nurses should think twice before using terms of endearment. Nursing Standard Royal College of Nursing, Volume 30(5), pp. 12 - 13.
Cooper, P., & Gray, D. (2001) Comparison of two skin care regimes for incontinence. British Journal of Nursing. Volume 10(6; Supplement) S6, S8, S10
Corcoran, L. (2005) Nutrition and hydration tips for stroke Patients with dysphagia. Nursing Times, Volume 101(48), pp.24 - 27.
Cott, C.A., Wiles, R., & Devitt, R. (2007) Continuity, transition and participation: preparing clients for life in the community post-stroke. Disability and Rehabilitation, Volume 29(20-21), pp.1566 - 1574.
Coulter, A., & Collins, A. (2011) Making shared decision-making a reality: No decision about me, without me. London: King’s Fund. http://www.kingsfund.org.uk/ publications/making-shared-decision-making-reality
Coulter, A., Fitzpatrick, R., & Cornwell, J. (2009). The Point of Care: measures of Patients’ experience in hospital: purpose, methods and uses. London: The King’s Fund. Available at: www.kingsfund.org. uk/sites/files/kf/Point-of-Care-Measures-of-Patients-experience-in-hospital-Kings-Fund-July-2009.pdf
Coulter, A., Roberts, S., & Dixon, A. (2013) Delivering better services for people with long-term conditions: Building the house of care, London: King’s Fund. http://www.kingsfund.org.uk/publications/delivering-better-services-peoplelong-term-conditions
Cullum, N., Deeks, J., Fletcher, A., Long, A., Mouneimne, H., Sheldon, T., & Song, F. (1995) The prevention and treatment of pressure sores: how effective are pressure-relieving interventions and risk assessment for the prevention and treatment of pressure sores. Effective Health Care, Volume 2(1), pp.1 - 16.
Cullum, N., Deeks, J., Sheldon, T., Song, F., & Fletcher, A. (2000) Beds, mattresses and cushions for pressure ulcer prevention and treatment. Cochrane Database of Systematic Reviews (2): CD001735. Update in Cochrane Database of Systematic Reviews 2004, 3: CD001735
Das, J., & Rajanikant, G.K. (2018) Post stroke depression: the sequelae of cerebral stroke. Neuroscience & Biobehavioral Reviews, Volume 90, pp.104 - 114.
Davis, K.J. (2006) Advocates: Qualities to look for and choosing the correct one for you. The Reporter. Volume 11(2). pp. 10 - 12.
Defloor, T., & Grypdonck, M.H. (1999) Sitting posture and prevention of pressure ulcers. Applied Nursing Research Volume 12(3), pp.136 – 142
DeJong, G., Horn, S.D., Conroy, B., Nichols, D., & Healton, E.B. (2005) Opening the black box of post-stroke rehabilitation: stroke rehabilitation Patients, processes, and outcomes. Archives of Physical Medicine and Rehabilitation, Volume 86(12), pp.1 - 7.
De Man‐van Ginkel, J.M., Gooskens, F., Schuurmans, M.J., Lindeman, E., Hafsteinsdottir, T.B. & Rehabilitation Guideline Stroke Working Group (2010) A systematic review of therapeutic interventions for post-stroke depression and the role of nurses. Journal of Clinical Nursing, Volume 19(23‐24), pp. 3274 - 3290.
de Man-van Ginkel, J.M., Hafsteinsdóttir, T.B., Lindeman, E., Ettema, R.G., Grobbee, D.E., & Schuurmans, M.J. (2013) In-hospital risk prediction for post-stroke depression: development and validation of the Post-stroke Depression Prediction Scale. Stroke, Volume 44(9), pp. 2441 - 2445.
De Saussure, F.M. (1916) Cours De Linguistique Générale. 5th Edition, Paris: Payout. English Translation by Baskin, W., i. New York: Philosophical Library, 1959
de Waal, A. ed. (2008) Inspecting the Inspectorate: Ofsted under scrutiny. Civitas Publishing
De Weerdt, D., & Kusters, A. (2016). Deaf space and the positioning of sign language interpreters. Kielisilta. 2016 (3), pp. 17-19.
Department of Health (1991). The Patient’s Charter. London: Her Majesty’s Stationery Office.
Department of Health (1989). Working for Patients. Cm 555. London: Her Majesty’s Stationery Office.
Dickerson, L. (1995) Techniques for the integration of people who use alternative communication devices in the workplace. 3rd Annual Pittsburgh Employment Conference. pp. 27 - 34. Pittsburgh: Shout Press
Dixon, A., Robertson, R., Appleby, J., Burge, P., Devlin, N., & Magee, H. (2010). Patient choice: how Patients choose and how providers respond. London: The King’s Fund. Available at: www.kingsfund.org.uk/ publications/Patient-choice
Dunbar, R. (1996) Grooming, gossip and the evolution of language. Faber and Faber ISBN 0-571-17396-9
Adigun, O.O., Mikhail, A.G., Krawiec, C., & Hatcher., J.D. (2020) Abuse and Neglect. StatPearls Publishing
Akyuz, G., & Kuru, P. (2016) Systematic review of central post stroke pain: what is happening in the central nervous system? American Journal of Physical Medicine & Rehabilitation, Volume 95(8), pp. 618 - 627.
Alcusky, M., Ulbricht, C.M., & Lapane, K.L. (2018) Post-acute care setting, facility characteristics, and post-stroke outcomes: a systematic review. Archives of Physical Medicine and Rehabilitation, Volume 99(6), pp.1124 - 1140.
Alderman, N. (2013) Managing challenging behaviour. In Neurobehavioural Disability and Social Handicap Following Traumatic Brain Injury. pp. 191 - 224. Psychology Press.
Allen, K., Hazelett, S., Jarjoura, D., Wright, K., Clough, L., & Weinhardt, J. (2004) Improving stroke outcomes: implementation of a post-discharge care management model. The Journal of Clinical Outcomes Management. Volume 11(11), pp. 707 - 717.
Allman, R.M. (1997) Pressure ulcer prevalence, incidence, risk factors, and impact. Clinics in Geriatric Medicine. Volume 13(3): pp. 421 – 436
Ancheta, J., Husband, M., Law, D., & Reding, M. (2000) Initial functional independence measure score and interval post stroke help assess outcome, length of hospitalization, and quality of care. Neurorehabilitation and Neural Repair, Volume 14(2), pp.127 - 134.
Andrewes, H.E., Walker, V., & O’Neill, B. (2014) Exploring the use of positive psychology interventions in brain injury survivors with challenging behaviour. Brain Injury, Volume 28(7), pp. 965 - 971.
Aziz, A.F.A., Nordin, N.A.M., Ali, M.F., Abd Aziz, N.A., Sulong, S. & Aljunid, S.M. (2017). The integrated care pathway for post stroke Patients (iCaPPS): a shared care approach between stakeholders in areas with limited access to specialist stroke care services. BMC Health Services Research, Volume 17(1), pp.1 - 11.
Aziz, A.F.A., Nordin, N.A.M., Abd Aziz, N., Abdullah, S., Sulong, S., & Aljunid, S.M. (2014) Care for post-stroke Patients at Malaysian public health centres: self-reported practices of family medicine specialists. BMC Family Practice, Volume 15(1), pp.1 - 11.
Bainbridge, L. (2019) .A Complete Guide on How to Use a Hoist Correctly https://www.beaucare.com/blog/a-complete-guide-on-how-to-use-a-hoist-for-correctly/
Bakas, T., Austin, J.K., Jessup, S.L., Williams, L.S., & Oberst, M.T. (2004) Time and difficulty of tasks provided by family caregivers of stroke survivors. Journal of Neuroscience Nursing, Volume 36(2), pp. 95 - 106.
Barlow J., Wright C., Sheasby J., Turner A., & Hainsworth, J. (2002) ‘Self-management approaches for people with chronic conditions: a review’, Patient Education and Counseling. Volume 48: pp. 177 - 187
Barton, A., & Barton, M. (1981) The Management and Prevention of Pressure Sores. Faber and Faber, London
Bastawrous, M., Gignac, M.A., Kapral, M.K. & Cameron, J.I. (2015) Adult daughters providing post-stroke care to a parent: a qualitative study of the impact that role overload has on lifestyle, participation and family relationships. Clinical Rehabilitation, Volume 29(6), pp.592 - 600.
Bastemeijer, C.M., Boosman, H., van Ewijk, H., Verweij, L.M., Voogt, L., & Hazelzet, J.A. (2019) Patient experiences: a systematic review of quality improvement interventions in a hospital setting. Patient Related Outcome Measures, Volume 10, pp.157 - 169.
Beamer, S. & Brookes, M. (2001) Making Decisions – best practice and new ideas for supporting people with high support needs to make decisions. Values Into Action. London
Berg, A., Palomaki, H., Lehtihalmes, M., Lönnqvist, J., & Kaste, M. (2003) Post-stroke depression: an 18-month follow-up. Stroke, Volume 34(1), pp.138 - 143.
Berger, S., Saut, A.M., & Berssaneti, F.T. (2020) Using Patient feedback to drive quality improvement in hospitals: a qualitative study. BMJ Open, Volume 10(10), p.e037641.
Bernstein, S. (2017) Don’t tell an upset person “calm down.” Do this instead. Web page article at: https://drsusanbernstein.com/dont-tell-an-upset-person-calm-down-%E2%80%8B-do-this-instead/
Birbeck Nevins, J. (1895) The sign language of the deaf and dumb. Proceedings of the Literary and Philosophical Society of Liverpool
Boden-Albala, B.M.P.H.D., Litwak, E., Elkind, M.S.V., Rundek, T.M.D.P., & Sacco, R.L. (2005) Social isolation and outcomes post-stroke. Neurology, Volume 64(11), pp.1888 - 1892.
Boivie, J. (2006) Central post-stroke pain. Handbook of Clinical Neurology, Volume 81, pp. 715 - 730.
Boosman, H., Schepers, V.P.M., Post, M.W.M., & Visser-Meily, J.M.A. (2011) Social activity contributes independently to life satisfaction three years post stroke. Clinical Rehabilitation, Volume 25(5), pp. 460 - 467.
Bowsher, D. (1995). The management of central post-stroke pain. Postgraduate Medical Journal, Volume 71(840), pp. 598 - 604.
Broomfield, N.M., Quinn, T.J., Abdul-Rahim, A.H., Walters, M.R., & N Evans, J.J. (2014) Depression and anxiety symptoms post-stroke/TIA: prevalence and associations in cross-sectional data from a regional stroke registry. BMC Neurology, Volume 14(1), pp. 1 - 9.
Brown, I., & Brown, R.I. (2003). Quality of Life and Disability.. Jessica Kingsley
Brown, I., & Brown, R.I. (2009). Choice as an aspect of quality of life for people with intellectual disabilities. Journal of Policy and Practice in Intellectual Disabilities, volume 6 (1), pp.11 - 18.
Bryen D.N. (1993) Augmentative Communication Mastery: One approach and some preliminary outcomes. The First Annual Pittsburgh
Employment Conference for Augmented Communicators Proceedings. August 20-22: Shout Press: Pittsburgh
Burns, S., & Day, T. (2012) A return to the basics: interventional Patient hygiene (a call for papers). Intensive and Critical Care Nursing; Volume 28(4), pp. 193 - 196.
Bustamante, A., Garcia-Berrocoso, T., Rodriguez, N., Llombart, V., Ribo, M., Molina, C. & Montaner, J. (2016) Ischemic stroke outcome: a review of the influence of post-stroke complications within the different scenarios of stroke care. European Journal of Internal Medicine, Volume 29, pp.9 - 21.
Cairns, D., Williams, V., Victor, C., Richards, S., Le May, A., Martin, W., & Oliver, D. (2013) The meaning and importance of dignified care: findings from a survey of health and social care professionals. BMC Geriatrics, Volume 13(1), pp. 1 - 6.
Cameron, J.I., Cheung, A.M., Streiner, D.L., Coyte, P.C., & Stewart, D.E. (2011) Stroke survivor depressive symptoms are associated with family caregiver depression during the first 2 years post-stroke. Stroke, Volume 42(2), pp.302 - 306.
Cameron, J.I., Stewart, D.E., Streiner, D.L., Coyte, P.C., & Cheung, A.M. (2014) What makes family caregivers happy during the first 2 years post stroke? Stroke, Volume 45(4), pp.1084 - 1089.
Campbell, G.B., & Matthews, J.T. (2010) An integrative review of factors associated with falls during post‐stroke rehabilitation. Journal of Nursing Scholarship, Volume 42(4), pp.395 - 404.
Caro, C.C., Mendes, P.V.B., Costa, J.D., Nock, L.J., & Cruz, D.M.C.D. (2017) Independence and cognition post-stroke and its relationship to burden and quality of life of family caregivers. Topics in Stroke Rehabilitation, Volume 24(3), pp. 194 - 199.
Cassidy, E.M., O'Connor, R., & O'Keane, V. (2004) Prevalence of post-stroke depression in an Irish sample and its relationship with disability and outcome following inPatient rehabilitation. Disability and Rehabilitation, Volume 26(2), pp. 71 - 77.
Chan, H. (1997) Bladder management in acute care of stroke patients: a quality improvement project. Journal of Neuroscience Nursing, Volume 29(3), pp. 187 - 191.
Choi‐Kwon, S., Choi, S.H., Suh, M., Choi, S., Cho, K.H., Nah, H.W., Song, H., & Kim, J.S. (2017) Musculoskeletal and central pain at 1 year post‐stroke: associated factors and impact on quality of life. Acta Neurologica Scandinavica, Volume 135(4), pp. 419 - 425.
Clarke, D.J., & Forster, A. (2015) Improving post-stroke recovery: the role of the multidisciplinary health care team. Journal of Multidisciplinary Healthcare, Volume 8, p. 433.
Clark, M., Defloor, T., & Bours, G. (2004) A pilot study of the prevalence of pressure ulcers in European hospitals. In: Clark, M., ed. Pressure Ulcers: Recent Advances in Tissue Viability. Quay Books, Salisbury: pp. 8 – 22
Clark, M., Schols, J., Benati, G., Jackson, P., & Engfer, M. (2004) Pressure ulcers and nutrition: a new European guideline. Journal of Wound Care. Volume 13(7): pp. 267 – 272
Cohen, D.L., Roffe, C., Beavan, J., Blackett, B., Fairfield, C.A., Hamdy, S., Havard, D., McFarlane, M., McLauglin, C., Randall, M., & Robson, K. (2016) Post-stroke dysphagia: a review and design considerations for future trials. International Journal of Stroke, Volume 11(4), pp. 399 - 411.
Collins, A. (2014). Measuring what really matters: towards a coherent measurement system to support person-centred care. London: The Health Foundation. Available at: www.health.org.uk/publications/ measuring-what-really-matters/
Collins, F. (2000) Selecting the most appropriate armchair for Patients. Journal of Wound Care. Volume 9(2): pp.73 – 76
Comerford, C. (2015). Why nurses should think twice before using terms of endearment. Nursing Standard Royal College of Nursing, Volume 30(5), pp. 12 - 13.
Cooper, P., & Gray, D. (2001) Comparison of two skin care regimes for incontinence. British Journal of Nursing. Volume 10(6; Supplement) S6, S8, S10
Corcoran, L. (2005) Nutrition and hydration tips for stroke Patients with dysphagia. Nursing Times, Volume 101(48), pp.24 - 27.
Cott, C.A., Wiles, R., & Devitt, R. (2007) Continuity, transition and participation: preparing clients for life in the community post-stroke. Disability and Rehabilitation, Volume 29(20-21), pp.1566 - 1574.
Coulter, A., & Collins, A. (2011) Making shared decision-making a reality: No decision about me, without me. London: King’s Fund. http://www.kingsfund.org.uk/ publications/making-shared-decision-making-reality
Coulter, A., Fitzpatrick, R., & Cornwell, J. (2009). The Point of Care: measures of Patients’ experience in hospital: purpose, methods and uses. London: The King’s Fund. Available at: www.kingsfund.org. uk/sites/files/kf/Point-of-Care-Measures-of-Patients-experience-in-hospital-Kings-Fund-July-2009.pdf
Coulter, A., Roberts, S., & Dixon, A. (2013) Delivering better services for people with long-term conditions: Building the house of care, London: King’s Fund. http://www.kingsfund.org.uk/publications/delivering-better-services-peoplelong-term-conditions
Cullum, N., Deeks, J., Fletcher, A., Long, A., Mouneimne, H., Sheldon, T., & Song, F. (1995) The prevention and treatment of pressure sores: how effective are pressure-relieving interventions and risk assessment for the prevention and treatment of pressure sores. Effective Health Care, Volume 2(1), pp.1 - 16.
Cullum, N., Deeks, J., Sheldon, T., Song, F., & Fletcher, A. (2000) Beds, mattresses and cushions for pressure ulcer prevention and treatment. Cochrane Database of Systematic Reviews (2): CD001735. Update in Cochrane Database of Systematic Reviews 2004, 3: CD001735
Das, J., & Rajanikant, G.K. (2018) Post stroke depression: the sequelae of cerebral stroke. Neuroscience & Biobehavioral Reviews, Volume 90, pp.104 - 114.
Davis, K.J. (2006) Advocates: Qualities to look for and choosing the correct one for you. The Reporter. Volume 11(2). pp. 10 - 12.
Defloor, T., & Grypdonck, M.H. (1999) Sitting posture and prevention of pressure ulcers. Applied Nursing Research Volume 12(3), pp.136 – 142
DeJong, G., Horn, S.D., Conroy, B., Nichols, D., & Healton, E.B. (2005) Opening the black box of post-stroke rehabilitation: stroke rehabilitation Patients, processes, and outcomes. Archives of Physical Medicine and Rehabilitation, Volume 86(12), pp.1 - 7.
De Man‐van Ginkel, J.M., Gooskens, F., Schuurmans, M.J., Lindeman, E., Hafsteinsdottir, T.B. & Rehabilitation Guideline Stroke Working Group (2010) A systematic review of therapeutic interventions for post-stroke depression and the role of nurses. Journal of Clinical Nursing, Volume 19(23‐24), pp. 3274 - 3290.
de Man-van Ginkel, J.M., Hafsteinsdóttir, T.B., Lindeman, E., Ettema, R.G., Grobbee, D.E., & Schuurmans, M.J. (2013) In-hospital risk prediction for post-stroke depression: development and validation of the Post-stroke Depression Prediction Scale. Stroke, Volume 44(9), pp. 2441 - 2445.
De Saussure, F.M. (1916) Cours De Linguistique Générale. 5th Edition, Paris: Payout. English Translation by Baskin, W., i. New York: Philosophical Library, 1959
de Waal, A. ed. (2008) Inspecting the Inspectorate: Ofsted under scrutiny. Civitas Publishing
De Weerdt, D., & Kusters, A. (2016). Deaf space and the positioning of sign language interpreters. Kielisilta. 2016 (3), pp. 17-19.
Department of Health (1991). The Patient’s Charter. London: Her Majesty’s Stationery Office.
Department of Health (1989). Working for Patients. Cm 555. London: Her Majesty’s Stationery Office.
Dickerson, L. (1995) Techniques for the integration of people who use alternative communication devices in the workplace. 3rd Annual Pittsburgh Employment Conference. pp. 27 - 34. Pittsburgh: Shout Press
Dixon, A., Robertson, R., Appleby, J., Burge, P., Devlin, N., & Magee, H. (2010). Patient choice: how Patients choose and how providers respond. London: The King’s Fund. Available at: www.kingsfund.org.uk/ publications/Patient-choice
Dunbar, R. (1996) Grooming, gossip and the evolution of language. Faber and Faber ISBN 0-571-17396-9
Edgman-Levitan, S., & Brady, C., with Howitt (2013) Partnering with Patients, Families, and Communities for Health: A Global Imperative. Report of the Family Engagement Working Group 2013, Doha: World Innovation Summit for Health. http://www.wish-qatar.org/app/media/387
Edwards, D.F., Hahn, M.G., Baum, C.M., Perlmutter, M.S., Sheedy, C., & Dromerick, A.W. (2006). Screening Patients with stroke for rehabilitation needs: validation of the post-stroke rehabilitation guidelines. Neurorehabilitation and Neural Repair, Volume 20(1), pp.42 - 48.
EPUAP (European Pressure Ulcer Advisory Panel) (1999) Guidelines on treatment of pressure ulcers. EPUAP Review Volume 1(2): pp. 31 – 33 (http://www.epuap.org/glprevention.html) (Last accessed 30 August 2005)
Foley, N., Teasell, R., Salter, K., Kruger, E., & Martino, R. (2008) Dysphagia treatment post stroke: a systematic review of randomised controlled trials. Age and Ageing, Volume 37(3), pp. 258 - 264.
Foot, C., Gilburt, H., Dunn, P., Jabbal, J., Seale, B., Goodrich, J., Buck, D., & Taylor, J. (2014) People in control of their own health and care: The state of involvement. The King’s Fund In association with National Voices
Formativ Health (2019) Putting the Patient in Charge. http://www.formativhealth.com/putting-the-Patient-in-charge/
Forster, A., Brown, L., Smith, J., House, A., Knapp, P., Wright, J.J., & Young, J. (2012). Information provision for stroke patients and their caregivers. Cochrane Database of Systematic Reviews, (11).
Gawande, A. (2009) Checklist Manifesto: How to Get Things Right, Metropolitan Books.
Gebhardt, K., & Bliss, M.R. (1994) Preventing pressure sores in orthopaedic Patients — is prolonged chair nursing detrimental? Journal of Tissue Viability Volume 4(2): pp. 51 – 54
Genet, N.B., Kringos, W.G., Bouman, D.S., Francke, A., Fagerström, A.L. Melchiorre, M., Greco, C., & Deville, W. (2011). Home care in Europe: a systematic literature review. BMC Health Services Research, Volume 11, p.207.
Glader, E.L., Stegmayr, B., & Asplund, K. (2002) Post-stroke fatigue: a 2-year follow-up study of stroke Patients in Sweden. Stroke, Volume 33(5), pp.1327 - 1333.
Gray, D., Cooper, P., & Clark, M. (1999) Pressure ulcer prevention in an acute hospital. Poster presentation, European Pressure Ulcer Advisory Panel (EPUAP), Amsterdam. EPUAP Review
Greene, J., & Hibbard J.H. (2012) ‘Why does Patient activation matter? An examination of the relationships between Patient activation and health-related outcomes’, Journal of General Internal Medicine. Volume 27(5): pp. 520 – 526
Gresham, G.E., Stason, W.B., & Duncan, P.W. (2004) Post-stroke rehabilitation (Volume 95, No. 662). Diane Publishing.
Hadidi, N., Treat-Jacobson, D.J., & Lindquist, R. (2009) Post-stroke depression and functional outcome: a critical review of literature. Heart & Lung, Volume 38(2), pp. 151 - 162.
Hammar, L.M., Alam, M., Olsen, M., Swall, A., & Boström, A.M. (2021) Being Treated With Respect and Dignity?—Perceptions of Home Care Service Among Persons With Dementia. Journal of the American Medical Directors Association, Volume 22(3), pp. 656 - 662.
Hansson, P. (2004) Post‐stroke pain case study: clinical characteristics, therapeutic options and long‐term follow‐up. European Journal of Neurology, Volume 11, pp. 22 - 30.
Harrison, M., Ryan, T., Gardiner, C., & Jones, A. (2017) Psychological and emotional needs, assessment, and support post-stroke: a multi-perspective qualitative study. Topics in Stroke Rehabilitation, Volume 24(2), pp.119 - 125.
Harrison, R.A., & Field, T.S. (2015) Post stroke pain: identification, assessment, and therapy. Cerebrovascular Diseases, Volume 39(3-4), pp.190 - 201.
Hartman-Maeir, A., Soroker, N., Ring, H., Avni, N., & Katz, N. (2007) Activities, participation and satisfaction one-year post stroke. Disability and Rehabilitation, Volume 29(7), pp. 559 - 566.
Haug, M., & Lavin, B. (1981). Practitioner or Patient - Who's in Charge? Journal of Health and Social Behaviour, Volume 22(3), pp. 212-229.
Health and Care Professions Council (2015) Preventing small problems from becoming big problems in health and care. Health and Care Professions Council (HCPC), Publication code: AUSTIN–PICKER15.
Available at - https://www.hcpc-uk.org/resources/reports/2015/preventing-small-problems-from-becoming-big-problems-in-health-and-care/
Health and Safety Executive (2011) Getting to grips with hoisting people. HSE information sheet; Health Services Information Sheet No 3. This document is available at www.hse.gov.uk/pubns/ hsis3.pdf.
Health Foundation. (2016) Person-centred care made simple: what everyone should know about person-centred care. London: Health Foundation.
Heaven, B., Bamford, C., May, C., & Moynihan, P. (2013). Food work and feeding assistance on hospital wards. Sociology of Health & Illness, Volume 35(4), pp. 628 - 642.
Henon, H. (2006) Pain after stroke: a neglected issue. Journal of Neurology, Neurosurgery & Psychiatry, Volume 77(5), pp. 569 - 569.
Herrmann, N., Seitz, D., Fischer, H., Saposnik, G., Calzavara, A., Anderson, G., & Rochon, P. (2011) Detection and treatment of post stroke depression: results from the registry of the Canadian stroke network. International Journal of Geriatric Psychiatry, Volume 26(11), pp. 1195 - 1200.
Herter, R., & Kazer, M.W. (2010) Best Practices in urinary catheter care. Home Healthcare Nurse. Volume 28(6): pp. 342 - 349.
Higgins, J. (2020) Promoting dignity in care. CPD Online College knowledge base. Available at - https://cpdonline.co.uk/knowledge-base/care/promoting-dignity-in-care/
Hogg, G., & Wilson, E. (2004) Does he take sugar? The disabled consumer and identity. In British Academy of Management Conference Proceedings. St. Andrews, Scotland.
Institute for Healthcare Improvement (2021) “Ask one question” challenge.
http://www.ihi.org/education/IHIOpenSchool/Chapters/Pages/AskOneQuestion.aspx
Jackendoff, R. (1972) Semantic interpretation in generative grammar. Cambridge, Mass.: MIT Press
Jackendoff, R. (1983) Semantics and cognition. Cambridge, Mass.: MIT Press
Jackendoff, R. (1987) The status of thematic relations in linguistic theory. Linguistic Inquiry, Volume 18, pp. 369 - 412
Jackendoff, R. (1987) Consciousness and the computational mind. Cambridge, MA: MIT Press
Jackendoff, R. (1990) Semantic structures. Cambridge, Mass.: MIT Press
Jackendoff, R.(1992) Languages of the mind. Cambridge, MA: MIT Press
Jackendoff, R. (1993) Patterns in the mind. Language and human nature. Harvester Wheatsheaf.
Jeffree, D., & McConkey, R. (1976) Let me speak. London: Human Horizons Series: Souvenir Press
Jensen, M.P., Chodroff, M.J., & Dworkin, R.H. (2007) The impact of neuropathic pain on health-related quality of life: review and implications. Neurology, Volume 68(15), pp. 1178 - 1182.
Jones, A.P. (1996) Impact. Liberator Ltd. Swinstead, Lincolnshire.
Jones, F. (2013) Self-management: is it time for a new direction in rehabilitation and post stroke care? Panminerva Medica, Volume 55(1), pp. 79 - 86.
Joseph, D. (1986) The morning. Communication Outlook. Volume 8 (2), Page 8
Kadowaki, L., Wister, A.V., & Chappell, N.L. (2015) Influence of home care on life satisfaction, loneliness, and perceived life stress. Canadian Journal on Aging/La Revue canadienne du vieillissement, Volume 34(1), pp. 75 - 89.
Katamba, F. (1994) English Words. London and New York: Routledge
Kenny, A. (1973) Wittgenstein. Allen Lane : The Penguin Press
Kiley, J. (2014) Why Punctuality is Important for Home Care Services in Fairfield, CT. Synergy HomeCare. Website page available at: https://www.synergyhomecare.com/agencies/ct/fairfield/ct05/blog/posts/2014/8/7/why-punctuality-is-important-for-home-care-services-in-fairfield-ct/
Kim, J.S. (2014) Pharmacological management of central post-stroke pain: a practical guide. CNS drugs, Volume 28(9), pp.787-797.
Kim, J.S. (2017) Management of post-stroke mood and emotional disturbances. Expert Review of Neurotherapeutics, Volume 17(12), pp. 1179 - 1188.
Kneebone, I.I., & Dunmore, E. (2000) Psychological management of post‐stroke depression. British Journal of Clinical Psychology, Volume 39(1), pp. 53 - 65.
Kneebone, I.I., & Lincoln, N.B. (2012) Psychological problems after stroke and their management: state of knowledge. Neuroscience & Medicine. Volume 3(01), pp.83 - 89.
Kong, K.H., & Young, S. (2000) Incidence and outcome of post-stroke urinary retention: a prospective study. Archives of Physical Medicine and Rehabilitation, Volume 81(11), pp. 1464 - 1467.
Kong, K.H., Woon, V.C, & Yang, S.Y. (2004) Prevalence of chronic pain and its impact on health-related quality of life in stroke survivors. Archives of Physical Medicine And Rehabilitation, Volume 85(1), pp. 35 - 40.
Kristensen, H.K., Tistad, M., Koch, L.V., & Ytterberg, C. (2016) The importance of patient involvement in stroke rehabilitation. PloS One, Volume 11(6), p.e0157149.
Kwok, C., McIntyre, A., Janzen, S., Mays, R., & Teasell, R. (2015) Oral care post stroke: a scoping review. Journal of Oral Rehabilitation, Volume 42(1), pp.65 - 74.
Kwon, M.J. (2017) The relationship between pain and quality of life in stroke Patients. Korean Society of Physical Medicine, Volume 12(2), pp. 83 - 90.
Langhorne, P., Stott, D.J., Robertson, L., MacDonald, J., Jones, L., McAlpine, C., Dick, F., Taylor, G.S., & Murray, G. (2000) Medical complications after stroke: a multicenter study. Stroke, Volume 31(6), pp. 1223 - 1229.
Laskowski-Jones, L. (2015) Terms of endearment? Nursing: Volume 45(5) p. 6
Lawton, S., & Shepherd, E. (2019) The underlying principles and procedure for bed bathing Patients. Nursing Times (online); Volume 115(5), pp. 45 - 47.
Lennon, S., McKenna, S., & Jones, F. (2013) Self-management programmes for people post stroke: a systematic review. Clinical Rehabilitation, Volume 27(10), pp.867 - 878.
Levenson, J.L., ed. (2000). Romeo and Juliet. The Oxford Shakespeare. Oxford: Oxford University Press
Light, J., McNaughton, D., & Parnes, P. (1986) A protocol for the assessment of the communicative interaction skills of nonspeaking severely handicapped adults and their facilitators. Toronto: Hugh Macmillan Medical Centre
Lurbe-Puerto, K., Leandro, M.E., & Baumann, M. (2012) Experiences of caregiving, satisfaction of life, and social repercussions among family caregivers, two years post-stroke. Social Work in Health Care, Volume 51(8), pp. 725 - 742.
MacKenzie, D., Creaser, G., Sponagle, K., Gubitz, G., MacDougall, P., Blacquiere, D., Miller, S., & Sarty, G. (2017) Best practice interprofessional stroke care collaboration and simulation: the student perspective. Journal of Interprofessional Care, Volume 31(6), pp. 793 - 796.
McBride, K.L., White, C.L., Sourial, R., & Mayo, N. (2004) Post-discharge nursing interventions for stroke survivors and their families. Journal of Advanced Nursing, Volume 47(2), pp. 192 - 200.
McDonald, C. (2014) Patients in control - why people with long-term conditions must be empowered. Institute for Public Policy Research
McInnes, E., (2004) The use of pressure relieving devices (beds, mattresses and overlays) for the prevention of pressure ulcers in primary and secondary care. Journal of Tissue Viability Volume 14(1): pp. 4–6
McLoughlin, I., Bayati-Bojakhi, S., Purushothaman, K., & Sohal, A. (2014) Informational requirements and client-centred disability care: Issues, problems and prospects in Australia. Social Policy and Society, Volume 13(4), p.609.
Mandliya, A., Das, A., Unnikrishnan, J.P., Amal, M.G., Sarma, P.S., & Sylaja, P.N. (2016) Post-stroke fatigue is an independent predictor of post-stroke disability and burden of care: a path analysis study. Topics in stroke rehabilitation, Volume 23(1), pp.1 - 7.
Mathus-Vliegen, E.M. (2004) Old age, malnutrition, and pressure sores: an ill-fated alliance. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences, Volume 59(4): pp.355 – 360
Mayo, N.E., Wood-Dauphinee, S., Cote, R., Durcan, L., & Carlton, J. (2002) Activity, participation, and quality of life 6 months post-stroke. Archives of Physical Medicine and Rehabilitation, Volume 83(8), pp.1035 - 1042.
Mental Capacity Act 2005 (Final edition 2007). Mental Capacity Act 2005: Code of practice. Department for Constitutional Affairs. London: The Stationery Office
Miller, M., & Glover, D. eds (1999) Wound Management Theory and Practice. Nursing Times Books, London
Min, J.H., Lee, S.E., Lee, H.S., Chae, Y.K., Lee, Y.K., Kang, Y., & Je, U.J. (2014) The correlation between the Trendelenburg position and the stroke volume variation. Korean Journal of Anesthesiology, Volume 67(6), pp. 378 – 383.
Mitchell, A.J., Sheth, B., Gill, J., Yadegarfar, M., Stubbs, B., Yadegarfar, M., & Meader, N. (2017) Prevalence and predictors of post-stroke mood disorders: A meta-analysis and meta-regression of depression, anxiety and adjustment disorder. General Hospital Psychiatry, 47, pp. 48 - 60.
Mitchell, P.H., Teri, L., Veith, R., Buzaitis, A., Tirschwell, D., Becker, K., Fruin, M., Kohen, R., & Cain, K.C. (2008) Living well with stroke: design and methods for a randomized controlled trial of a psychosocial behavioural intervention for post-stroke depression. Journal of Stroke and Cerebrovascular Diseases, Volume 17(3), pp.109 - 115.
Mulla, S.M., Wang, L., Khokhar, R., Izhar, Z., Agarwal, A., Couban, R., Buckley, D.N., Moulin, D.E., Panju, A., Makosso-Kallyth, S., & Turan, A. (2015) Management of central post-stroke pain: systematic review of randomized controlled trials. Stroke, Volume 46(10), pp. 2853 - 2860.
Mulley, A., Trimble, C., & Elwyn, G. (2012). Patients’ preferences matter: stop the silent misdiagnosis. London: The King’s Fund. Available at: www.kingsfund.org.uk/publications/Patients-preferencesmatter
Myers, B. (2019) Are Too Many Choices Leaving Your Patients Dazed and Confused? Audiology Today. November/December 2019, page 8
Nagasaka, K., Takashima, I., Matsuda, K., & Higo, N. (2017) Late-onset hypersensitivity after a lesion in the ventral posterolateral nucleus of the thalamus: a macaque model of central post-stroke pain. Scientific Reports, Volume 7(1), pp. 1 - 12.
Neal-Boylan, L. (2006) The rehabilitation nurse specialist in home care. Home Healthcare Now, Volume 24(7), pp. 457 - 458.
Niedermaier, N., Bohrer, E., Schulte, K., Schlattmann, P., & Heuser, I. (2004) Prevention and treatment of post-stroke depression with mirtazapine in Patients with acute stroke. Journal of Clinical Psychiatry, Volume 65(12), pp. 1619 - 1623.
Oakley, M. (1991) Quoted in ‘The Hidden Handicap’ by Darby, S. Times Educational Supplement (No.3930) October 25 1991 page 38
Olaison, A. (2017) Processing older persons as clients in elderly care: A study of the micro-processes of care management practice. Social Work in Health Care, Volume 56(2), pp. 78 - 98.
Opara, J.A., & Jaracz, K. (2010) Quality of life of post–stroke Patients and their caregivers. Journal of Medicine and Life, Volume 3(3), p. 216.
Parikh, R.M., Eden, D.T., Price, T.R., & Robinson, R.G. (1989) The sensitivity and specificity of the Center for Epidemiologic Studies Depression Scale in screening for post-stroke depression. The International Journal of Psychiatry in Medicine, Volume 18(2), pp.169 - 181.
Parikh, R.M., Robinson, R.G., Lipsey, J.R., Starkstein, S.E., Fedoroff, J.P., & Price, T.R. (1990) The impact of post-stroke depression on recovery in activities of daily living over a 2-year follow-up. Archives of Neurology, Volume 47(7), pp.785 - 789.
Payton, H. & Soundy, A. (2020) The Experience of Post-Stroke Pain and the Impact on Quality of Life: An Integrative Review. Behavioural Sciences, Volume 10(8), pp. 128- .
Pepe, P.E., Zachariah, B.S., Sayre, M.R., Floccare, D., & Writing, R. (1998) Ensuring the chain of recovery for stroke in your community. Prehospital Emergency Care, Volume 2(2), pp. 89 - 95.
Perry, L. (2001) Screening swallowing function of patients with acute stroke. Part two: Detailed evaluation of the tool used by nurses. Journal of Clinical Nursing, Volume 10(4), pp. 474 - 481.
Philp, I., Brainin, M., Walker, M.F., Ward, A.B., Gillard, P., Shields, A.L., Norrving, B. & Panel, G.S.C.A. (2013) Development of a post-stroke checklist to standardize follow-up care for stroke survivors. Journal of Stroke and Cerebrovascular Diseases, Volume 22(7), pp.173 - 180.
Pinker, S. (1994) The language instinct. First published by William Morrow and Co. Penguin Press: ISBN 0-14-017529-6
Piron, L., Turolla, A., Tonin, P., Piccione, F., Lain, L. & Dam, M. (2008) Satisfaction with care in post-stroke Patients undergoing a telerehabilitation programme at home. Journal of Telemedicine and Telecare, Volume 14(5), pp.257 - 260.
Pohjasvaara, T., Vataja, R., Leppävuori, A., Kaste, M., & Erkinjuntti, T. (2001) Depression is an independent predictor of poor long‐term functional outcome post‐stroke. European Journal of Neurology, Volume 8(4), pp. 315 - 319.
Raab, K. (2014) Mindfulness, self-compassion, and empathy among health care professionals: a review of the literature. Journal of Health Care Chaplaincy, Volume 20(3), pp. 95 - 108.
Rajsic, S., Gothe, H., Borba, H.H., Sroczynski, G., Vujicic, J., Toell, T. & Siebert, U. (2019). Economic burden of stroke: a systematic review on post-stroke care. The European Journal of Health Economics, Volume 20(1), pp.107 - 134.
Reddy, M., Keast, D., Fowler, E. & Sibbald, R.G. (2003) Pain in pressure ulcers. Ostomy/wound management, Volume 49(4 Supplement) pp.30 - 35.
Robison, J., Wiles, R., Ellis-Hill, C., McPherson, K., Hyndman, D., & Ashburn, A. (2009) Resuming previously valued activities post-stroke: who or what helps? Disability and Rehabilitation, Volume 31(19), pp.1555 - 1566.
Rochette, A., Korner-Bitensky, N., & Desrosiers, J. (2007) Actual vs best practice for families post-stroke according to three rehabilitation disciplines. Journal of Rehabilitation Medicine, Volume 39(7), pp. 513 - 519.
Rodeheaver, G.T. (1999) Pressure ulcer debridement and cleansing: a review of current literature. Ostomy/Wound Management Volume 45 (1A Supplement) pp. 80 – 85
Romanelli, M., & Mastronicola, D. (2002) The role of wound-bed preparation in managing chronic pressure ulcers. Journal of Wound Care Volume 11(8): pp. 305 –310
Rubin, M.N., Wellik, K.E., Channer, D.D. & Demaerschalk, B.M. (2013) Systematic review of telestroke for post-stroke care and rehabilitation. Current atherosclerosis reports, Volume 15(8), pp.1 - 7.
Ryden, M.B., & Knopman, D. (1989) Assess not assume: measuring the morale of cognitively impaired elderly. Journal of Gerontological Nursing. Volume 15(11), pp.27 - 32.
Sacks, O. (1985) The man who mistook his wife for a hat. New York: Summit Books
Sacks, O. (1989) Seeing Voices University of California press. Picador Edition (1991) ISBN 0-330-31716-4
Sacks, O. (1994) A Neurologist’s Notebook. An Anthropologist on Mars. New Yorker, LXIX, 44, December 27, 106‑125
Şahin-Onat, Ş., Ünsal-Delialioğlu, S., Kulaklı, F., & Özel, S. (2016) The effects of central post-stroke pain on quality of life and depression in Patients with stroke. Journal of Physical Therapy Science, Volume 28(1), pp. 96 - 101.
Salter, K., Andrew McClure, J., Mahon, H., Foley, N., & Teasell, R. (2012) Adherence to Canadian best practice recommendations for stroke care: assessment and management of post-stroke depression in an Ontario rehabilitation facility. Topics in Stroke Rehabilitation, Volume 19(2), pp.132 - 140.
Sandberg, L., Nilsson, I., Rosenberg, L., Borell, L., & Boström, A.M. (2019) Home care services for older clients with and without cognitive impairment in Sweden. Health & Social Care in the Community, Volume 27(1), pp. 139 - 150.
Sarfo, F.S., Jenkins, C., Singh, A., Owolabi, M., Ojagbemi, A., Adusei, N., Saulson, R., & Ovbiagele, B. (2017) Post-stroke depression in Ghana: characteristics and correlates. Journal of the Neurological Sciences, Volume 379, pp. 261 - 265.
Schmid, A.A., Kroenke, K., Hendrie, H.C., Bakas, T., Sutherland, J.M., & Williams, L.S. (2011) Post-stroke depression and treatment effects on functional outcomes. Neurology, Volume 76(11), pp.1000 - 1005.
Schoot, T., Proot, I., Meulen, R.T., & de Witte, L. (2005) Recognition of client values as a basis for tailored care: the view of Dutch expert Patients and family caregivers. Scandinavian Journal of Caring Sciences, Volume 19(2), pp. 169 - 176.
Sienkiewicz-Mercer, R. & Kaplan, S.B. (1989) I raise my eyes to say yes. Houghton Mifflin
Smith, L.N., Norrie, J., Kerr, S.M., Lawrence, I.M., Langhorne, P., & Lees, K.R. (2004) Impact and influences on caregiver outcomes at one year post-stroke. Cerebrovascular Diseases, Volume 18(2), pp.145 - 153.
Srivastava, A., Taly, A.B., Gupta, A. & Murali, T. (2010) Post-stroke depression: prevalence and relationship with disability in chronic stroke survivors. Annals of Indian Academy of Neurology, Volume 13(2), p.123.
Sulch, D., Melbourn, A., Perez, I., & Kalra, L. (2002) Integrated care pathways and quality of life on a stroke rehabilitation unit. Stroke, Volume 33(6), pp. 1600 - 1604.
Summers, D., Leonard, A., Wentworth, D., Saver, J.L., Simpson, J., Spilker, J.A., Hock, N., Miller, E., & Mitchell, P.H. (2009) Comprehensive overview of nursing and interdisciplinary care of the acute ischemic stroke patient: a scientific statement from the American Heart Association. Stroke, Volume 40(8), pp. 2911 - 2944.
Svenaeus, F. (2015) The relationship between empathy and sympathy in good health care. Medicine, Health Care and Philosophy, Volume 18(2), pp. 267 - 277.
Sterr, A., Kuhn, M., Nissen, C., Ettine, D., Funk, S., Feige, B., Umarova, R., Urbach, H., Weiller, C. & Riemann, D. (2018) Post-stroke insomnia in community-dwelling Patients with chronic motor stroke: Physiological evidence and implications for stroke care. Scientific reports, Volume 8(1), pp.1-9.
Stotts, N.A., Rodeheaver, G.T. & Thomas, D.R., Frantz, R.A., Bartolucci, A.A., Sussman, C., Ferrell, B.A., Cuddigan, J., & Maklebust, J. (2001) An instrument to measure healing in pressure ulcers: development and validation of the pressure ulcer scale for healing (PUSH). The Journals of Gerontology Series A: Biological Sciences and Medical Sciences, Volume 56(12): pp. 795 – 799
Suh, M., Kim, K., Kim, I., Cho, N., Choi, H., & Noh, S. (2005) Caregiver's burden, depression and support as predictors of post-stroke depression: a cross-sectional survey. International Journal of Nursing Studies, Volume 42(6), pp. 611 - 618.
Tasa, K., Baker, G.R. and Murray, M. (1996) Using Patient Feedback for Quality. Quality Management in Health Care, Volume 4(2), pp. 55 - 67.
The Times (2016) Careless Care: If the dignity of the elderly is to be respected, social care needs urgent reform. Leading Article, The Times, Thursday, November 10, 2016.
Towfighi, A., Ovbiagele, B., El Husseini, N., Hackett, M.L., Jorge, R.E., Kissela, B.M., Mitchell, P.H., Skolarus, L.E., Whooley, M.A., & Williams, L.S. (2017) Poststroke depression: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke, Volume 48(2), pp.e30 - e43.
Trask, R.L. (1994) Language change. London: Routledge
Trask, R.L. (1995) Language - The basics. London: Routledge
Twine, F. (1994). Citizenship ans Social Rights: The interdependence of self and society. London: Sage Publications
Van de Weg, F.B., Kuik, D.J., & Lankhorst, G.J. (1999) Post-stroke depression and functional outcome: a cohort study investigating the influence of depression on functional recovery from stroke. Clinical Rehabilitation, Volume 13(3), pp. 268 - 272.
Van Mierlo, M.L., Van Heugten, C.M., Post, M.W., Hajos, T.R., Kappelle, L.J., Visser-Meily, J.M. (2016) Quality of life during the first two years post stroke: the Restore4Stroke cohort study. Cerebrovascular Diseases, Volume 41(1-2), pp.19 - 26.
Vatwani, A. (2017) Caregiver Guide and Instructions for Safe Bed Mobility. Archives of Physical Medicine and Rehabilitation, Volume 98(9), pp. 1907 - 1910.
Veatch, R.M. (2008) Patient, Heal Thyself: How the New Medicine Puts the Patient in Charge, Oxford University Press
Veerbeek, J.M., van Wegen, E., van Peppen, R., van der Wees, P.J., Hendriks, E., Rietberg, M., & Kwakkel, G. (2014) What is the evidence for physical therapy post-stroke? A systematic review and meta-analysis. PloS one, Volume 9(2), p. e87987.
Visser-Meily, A., Post, M., van de Port, I., Maas, C., Forstberg-Wärleby, G., & Lindeman, E. (2009) Psychosocial functioning of spouses of Patients with stroke from initial inPatient rehabilitation to 3 years post-stroke: course and relations with coping strategies. Stroke, Volume 40(4), pp.1399 - 1404.
Wagner, M.G. (1991). Does he take sugar? World health forum; Volume 12(1) : pp, 87 - 89 https://apps.who.int/iris/handle/10665/49206
Ward, H.O., Kibble, S., Mehta, G., Franklin, M., Kovoor, J., Jones, A., Panesar, S., & Carson-Stevens A. (2013) How Asking Patients a Simple Question Enhances Care at the Bedside: Medical Students as Agents of Quality Improvement. The Permanente Journal, Volume 17(4): pp. 27 – 31.
Ware, J. (2012) Creating a responsive environment for people with profound and multiple learning difficulties. Routledge.
Watret, L. (1999) Using a case-mix-adjusted pressure sore incidence study in a surgical directorate to improve Patient outcomes in pressure ulcer prevention. Journal of Tissue Viability Volume 9(4): pp. 121 – 125
Wensing, M., Vingerhoets, E., & Grol, R. (2003) Feedback based on Patient evaluations: a tool for quality improvement? Patient Education and Counselling, Volume 51(2), pp. 149 - 153.
Westendorp, W.F., Nederkoorn, P.J., Vermeij, J.D., Dijkgraaf, M.G. & van de Beek, D. (2011) Post-stroke infection: a systematic review and meta-analysis. BMC Neurology, Volume 11(1), pp.1 - 7.
Widar, M., Ek, A.C., & Ahlström, G. (2007) Caring and uncaring experiences as narrated by persons with long‐term pain after a stroke. Scandinavian Journal of Caring sciences, Volume 21(1), pp. 41 - 47.
Wissel, J., Olver, J., & Sunnerhagen, K.S. (2013) Navigating the post-stroke continuum of care. Journal of Stroke and Cerebrovascular Diseases, Volume 22(1), pp.1 - 8.
Wittgenstein, L.J.J. (1953) Philosophische Untersuchungen. English Translation by Ainscombe G. Oxford University Press 1958.
Wolff, A.M., Taylor, S.A., & McCabe, J.F. (2004) Using checklists and reminders in clinical pathways to improve hospital inpatient care. Medical Journal of Australia, Volume 181(8), pp. 428 - 431.
Yoon, P.S., Ooi, C.H., & How, C.H. (2018) Approach to the forgetful Patient. Singapore Medical Journal, Volume 59(3), p.121 – 125.
Young, T. (2004) The 30 degree tilt position vs the 90 degree lateral and supine positions in reducing the incidence of non-blanching erythema in a hospital inPatient population: a randomised controlled trial. Journal of Tissue Viability Volume 14(3): pp. 88 – 96
Sacks, O. (1989) Seeing Voices University of California press. Picador Edition (1991) ISBN 0-330-31716-4
Sacks, O. (1994) A Neurologist’s Notebook. An Anthropologist on Mars. New Yorker, LXIX, 44, December 27, 106‑125
Şahin-Onat, Ş., Ünsal-Delialioğlu, S., Kulaklı, F., & Özel, S. (2016) The effects of central post-stroke pain on quality of life and depression in Patients with stroke. Journal of Physical Therapy Science, Volume 28(1), pp. 96 - 101.
Salter, K., Andrew McClure, J., Mahon, H., Foley, N., & Teasell, R. (2012) Adherence to Canadian best practice recommendations for stroke care: assessment and management of post-stroke depression in an Ontario rehabilitation facility. Topics in Stroke Rehabilitation, Volume 19(2), pp.132 - 140.
Sandberg, L., Nilsson, I., Rosenberg, L., Borell, L., & Boström, A.M. (2019) Home care services for older clients with and without cognitive impairment in Sweden. Health & Social Care in the Community, Volume 27(1), pp. 139 - 150.
Sarfo, F.S., Jenkins, C., Singh, A., Owolabi, M., Ojagbemi, A., Adusei, N., Saulson, R., & Ovbiagele, B. (2017) Post-stroke depression in Ghana: characteristics and correlates. Journal of the Neurological Sciences, Volume 379, pp. 261 - 265.
Schmid, A.A., Kroenke, K., Hendrie, H.C., Bakas, T., Sutherland, J.M., & Williams, L.S. (2011) Post-stroke depression and treatment effects on functional outcomes. Neurology, Volume 76(11), pp.1000 - 1005.
Schoot, T., Proot, I., Meulen, R.T., & de Witte, L. (2005) Recognition of client values as a basis for tailored care: the view of Dutch expert Patients and family caregivers. Scandinavian Journal of Caring Sciences, Volume 19(2), pp. 169 - 176.
Sienkiewicz-Mercer, R. & Kaplan, S.B. (1989) I raise my eyes to say yes. Houghton Mifflin
Smith, L.N., Norrie, J., Kerr, S.M., Lawrence, I.M., Langhorne, P., & Lees, K.R. (2004) Impact and influences on caregiver outcomes at one year post-stroke. Cerebrovascular Diseases, Volume 18(2), pp.145 - 153.
Srivastava, A., Taly, A.B., Gupta, A. & Murali, T. (2010) Post-stroke depression: prevalence and relationship with disability in chronic stroke survivors. Annals of Indian Academy of Neurology, Volume 13(2), p.123.
Sulch, D., Melbourn, A., Perez, I., & Kalra, L. (2002) Integrated care pathways and quality of life on a stroke rehabilitation unit. Stroke, Volume 33(6), pp. 1600 - 1604.
Summers, D., Leonard, A., Wentworth, D., Saver, J.L., Simpson, J., Spilker, J.A., Hock, N., Miller, E., & Mitchell, P.H. (2009) Comprehensive overview of nursing and interdisciplinary care of the acute ischemic stroke patient: a scientific statement from the American Heart Association. Stroke, Volume 40(8), pp. 2911 - 2944.
Svenaeus, F. (2015) The relationship between empathy and sympathy in good health care. Medicine, Health Care and Philosophy, Volume 18(2), pp. 267 - 277.
Sterr, A., Kuhn, M., Nissen, C., Ettine, D., Funk, S., Feige, B., Umarova, R., Urbach, H., Weiller, C. & Riemann, D. (2018) Post-stroke insomnia in community-dwelling Patients with chronic motor stroke: Physiological evidence and implications for stroke care. Scientific reports, Volume 8(1), pp.1-9.
Stotts, N.A., Rodeheaver, G.T. & Thomas, D.R., Frantz, R.A., Bartolucci, A.A., Sussman, C., Ferrell, B.A., Cuddigan, J., & Maklebust, J. (2001) An instrument to measure healing in pressure ulcers: development and validation of the pressure ulcer scale for healing (PUSH). The Journals of Gerontology Series A: Biological Sciences and Medical Sciences, Volume 56(12): pp. 795 – 799
Suh, M., Kim, K., Kim, I., Cho, N., Choi, H., & Noh, S. (2005) Caregiver's burden, depression and support as predictors of post-stroke depression: a cross-sectional survey. International Journal of Nursing Studies, Volume 42(6), pp. 611 - 618.
Tasa, K., Baker, G.R. and Murray, M. (1996) Using Patient Feedback for Quality. Quality Management in Health Care, Volume 4(2), pp. 55 - 67.
The Times (2016) Careless Care: If the dignity of the elderly is to be respected, social care needs urgent reform. Leading Article, The Times, Thursday, November 10, 2016.
Towfighi, A., Ovbiagele, B., El Husseini, N., Hackett, M.L., Jorge, R.E., Kissela, B.M., Mitchell, P.H., Skolarus, L.E., Whooley, M.A., & Williams, L.S. (2017) Poststroke depression: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke, Volume 48(2), pp.e30 - e43.
Trask, R.L. (1994) Language change. London: Routledge
Trask, R.L. (1995) Language - The basics. London: Routledge
Twine, F. (1994). Citizenship ans Social Rights: The interdependence of self and society. London: Sage Publications
Van de Weg, F.B., Kuik, D.J., & Lankhorst, G.J. (1999) Post-stroke depression and functional outcome: a cohort study investigating the influence of depression on functional recovery from stroke. Clinical Rehabilitation, Volume 13(3), pp. 268 - 272.
Van Mierlo, M.L., Van Heugten, C.M., Post, M.W., Hajos, T.R., Kappelle, L.J., Visser-Meily, J.M. (2016) Quality of life during the first two years post stroke: the Restore4Stroke cohort study. Cerebrovascular Diseases, Volume 41(1-2), pp.19 - 26.
Vatwani, A. (2017) Caregiver Guide and Instructions for Safe Bed Mobility. Archives of Physical Medicine and Rehabilitation, Volume 98(9), pp. 1907 - 1910.
Veatch, R.M. (2008) Patient, Heal Thyself: How the New Medicine Puts the Patient in Charge, Oxford University Press
Veerbeek, J.M., van Wegen, E., van Peppen, R., van der Wees, P.J., Hendriks, E., Rietberg, M., & Kwakkel, G. (2014) What is the evidence for physical therapy post-stroke? A systematic review and meta-analysis. PloS one, Volume 9(2), p. e87987.
Visser-Meily, A., Post, M., van de Port, I., Maas, C., Forstberg-Wärleby, G., & Lindeman, E. (2009) Psychosocial functioning of spouses of Patients with stroke from initial inPatient rehabilitation to 3 years post-stroke: course and relations with coping strategies. Stroke, Volume 40(4), pp.1399 - 1404.
Wagner, M.G. (1991). Does he take sugar? World health forum; Volume 12(1) : pp, 87 - 89 https://apps.who.int/iris/handle/10665/49206
Ward, H.O., Kibble, S., Mehta, G., Franklin, M., Kovoor, J., Jones, A., Panesar, S., & Carson-Stevens A. (2013) How Asking Patients a Simple Question Enhances Care at the Bedside: Medical Students as Agents of Quality Improvement. The Permanente Journal, Volume 17(4): pp. 27 – 31.
Ware, J. (2012) Creating a responsive environment for people with profound and multiple learning difficulties. Routledge.
Watret, L. (1999) Using a case-mix-adjusted pressure sore incidence study in a surgical directorate to improve Patient outcomes in pressure ulcer prevention. Journal of Tissue Viability Volume 9(4): pp. 121 – 125
Wensing, M., Vingerhoets, E., & Grol, R. (2003) Feedback based on Patient evaluations: a tool for quality improvement? Patient Education and Counselling, Volume 51(2), pp. 149 - 153.
Westendorp, W.F., Nederkoorn, P.J., Vermeij, J.D., Dijkgraaf, M.G. & van de Beek, D. (2011) Post-stroke infection: a systematic review and meta-analysis. BMC Neurology, Volume 11(1), pp.1 - 7.
Widar, M., Ek, A.C., & Ahlström, G. (2007) Caring and uncaring experiences as narrated by persons with long‐term pain after a stroke. Scandinavian Journal of Caring sciences, Volume 21(1), pp. 41 - 47.
Wissel, J., Olver, J., & Sunnerhagen, K.S. (2013) Navigating the post-stroke continuum of care. Journal of Stroke and Cerebrovascular Diseases, Volume 22(1), pp.1 - 8.
Wittgenstein, L.J.J. (1953) Philosophische Untersuchungen. English Translation by Ainscombe G. Oxford University Press 1958.
Wolff, A.M., Taylor, S.A., & McCabe, J.F. (2004) Using checklists and reminders in clinical pathways to improve hospital inpatient care. Medical Journal of Australia, Volume 181(8), pp. 428 - 431.
Yoon, P.S., Ooi, C.H., & How, C.H. (2018) Approach to the forgetful Patient. Singapore Medical Journal, Volume 59(3), p.121 – 125.
Young, T. (2004) The 30 degree tilt position vs the 90 degree lateral and supine positions in reducing the incidence of non-blanching erythema in a hospital inPatient population: a randomised controlled trial. Journal of Tissue Viability Volume 14(3): pp. 88 – 96
 Download Paper
Download Paper
To download this paper please click on the button left.
If you would like to comment on any aspect of this page
please use the form below.

Return to the top of this page
Click on the Up Key left

Return to the Main Page
Click on the Back Key left